 “I’m not sure I agree with that!”
“I’m not sure I agree with that!”
“I’ve got a funny feeling in my belly.”
“I better watch out!”
Theories of consciousness must run through the body. How integrated are the organs of the human body with the embodied mind? Are specific organs, like the heart and the gut, critical to emotions, unconscious decision-making, memory, and the general function of consciousness?
The gut, the center of gravity of the body, the “core” in athletic training, the focus of life sustaining eating and drinking, has the second largest brain in the human body with the least control from the higher brain centers. This “second brain” has been considered important in intuitive reasoning, intuition commonly referred to as “gut feelings”. The gut has important roles in our experiences of fear, anxiety, anticipation, and other important emotions.
Now, the trillions of microbes in the gut, ten times more cells that the total of human cells, have been called the “forgotten organ.” These microbes with a vast number of genes have great influence in the gut and on the brain (see previous post).
Recently, the question has become the importance of the Brain-Gut-Microbe axis.
The Second Brain
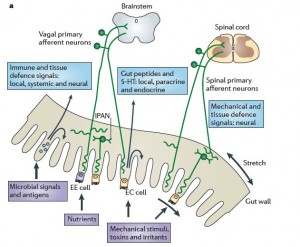
The gut nervous system and the brain are in constant communication. Unlike many parts of the body, the gut has a large, complex, semi-autonomous brain, housing more serotonin neurons than the rest of the brain. It makes the most independent decisions of any part of the anatomy and its endocrine signaling to the entire body is very elaborate
Communication from the gut to the anterior cingulate, orbitofrontal cortex and the amygdala has important effects on emotions, motivation and cognition. There is increasing evidence that signals from the microbes in the gut also affect memory, emotions and behavior in these same brain regions.
 The two major branches of the autonomic nervous system, the sympathetic and parasympathetic, are intimately tied to all the visceral organs, such as the gut, heart, lungs, and the kidneys, and are also very connected to
The two major branches of the autonomic nervous system, the sympathetic and parasympathetic, are intimately tied to all the visceral organs, such as the gut, heart, lungs, and the kidneys, and are also very connected to 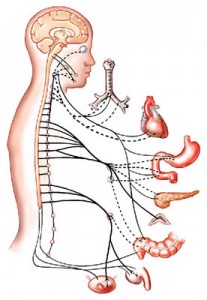 emotions. Only a very small part of this enormous innervation is perceived consciously, such as those circuits used for eating and bowel movements.
emotions. Only a very small part of this enormous innervation is perceived consciously, such as those circuits used for eating and bowel movements.
While there are 10 trillion total human cells, 100 trillion microbes live in the gut. Microbes in the gut have 150 times the number of unique genes compared with human cells (3.3 million microbe genes in the human), while sending signals inside the human being.
Microbes affect anxiety, mood, cognition and pain. Mechanisms include changes in the types of microbes present in the gut, activation of immune activity (discussed in previous post on Nervous and Immune Systems), nervous system signals through the vagus and sympathetic neurons, and specific metabolic products of microbes and gut cells including neurotransmitters and cell wall sugars.
The Forgotten Organ
 The 100 trillion microbes in the gut (most in the lower gut) have been referred to as the “forgotten organ”. Because most of the microbes in the gut are anaerobes, they have not been able to be cultivated in the laboratory for studies, but are now known to be critical in development of the fetus, as well as the innate and adaptive immune systems. These microbes are involved in regulating gut motility, nutrient absorption, and fat distribution.
The 100 trillion microbes in the gut (most in the lower gut) have been referred to as the “forgotten organ”. Because most of the microbes in the gut are anaerobes, they have not been able to be cultivated in the laboratory for studies, but are now known to be critical in development of the fetus, as well as the innate and adaptive immune systems. These microbes are involved in regulating gut motility, nutrient absorption, and fat distribution.
Each person has a dominant microbe strain and a balanced composition that appears to correlate with health. The two primary bacteria in normal guts are Bacteroidetes and Firmicutes with smaller amounts of Proteobacteria, Actinobacteria, Fusobacteria.
After a natural delivery when the newborn is essentially germ free, more than 1000 species and 7000 strains of microbes commence living in the baby’s gut. These strains are most often very similar to the mother.
Diet has a major effect on the composition of the microbes. For example, Bacteroides occur with high fat or protein, whereas the Prevotella are associated with high-carbohydrate.
Interestingly, the core microbiota in the elderly has been reported to be different from that of younger adult, and its composition is directly correlated with health outcomes.
Neurons in the Gut
While the gut has the largest nervous system outside the brain, with many local ganglion and plexus, there are only a small number of bidirectional neuronal connections between the gut and the brain.
 As noted above, the major connections are through the autonomic nervous system, that is, the sympathetic and parasympathetic. Both the sympathetic (adrenaline – fight and flight) nervous system and the parasympathetic (rest, dreaming, rebuilding – acetylcholine) are important in emotions and were highlighted in the posts on sleep, dreaming, body consciousness and spiritual experiences. The spinal reflexes and the nerves in the hypothalamic adrenal pathways are very important in both immune and emotional systems and communicate with the hypothalamus and amygdala
As noted above, the major connections are through the autonomic nervous system, that is, the sympathetic and parasympathetic. Both the sympathetic (adrenaline – fight and flight) nervous system and the parasympathetic (rest, dreaming, rebuilding – acetylcholine) are important in emotions and were highlighted in the posts on sleep, dreaming, body consciousness and spiritual experiences. The spinal reflexes and the nerves in the hypothalamic adrenal pathways are very important in both immune and emotional systems and communicate with the hypothalamus and amygdala
Brain gut interactions have been associated with eating disorders, chronic gut pain and inflammation disorders. It is now clear that alterations in brain–gut interactions are associated with gut inflammation, and are highly correlated with stress reactions and behavior. There is a high association between stress, anxiety and gut disorders such as irritable bowel syndrome.
Microbes and the Gut-Brain Connection
Crucially, microbes vitally affect the bidirectional influences of the gut and the brain.
 In a previous post, it was shown that microbes from the gut can send factors to the brain, which stimulate BDNF and other signals to make new brain cells, or otherwise. These signals are part of a large network of endocrine cells in the gut sending signals into the blood. These signals can effect the huge vagus nerve and effect changes in the brain. They also regulate local GI function.
In a previous post, it was shown that microbes from the gut can send factors to the brain, which stimulate BDNF and other signals to make new brain cells, or otherwise. These signals are part of a large network of endocrine cells in the gut sending signals into the blood. These signals can effect the huge vagus nerve and effect changes in the brain. They also regulate local GI function.
Also the immune system is critical in relaying information to the brain (see post on Nervous and Immune Systems). Seventy five percent of the body’s immune cells are in the gut. The immune system is deliberately less responsive the trillions of microbes in residence. But, somehow can become instantly alert when one of these communities changes into an aggressive variant. These interact with the endocrine cells and signals. The cells give a tonic response to the friendly microbes.
Many Mechanisms of Microbe Influence
The mechanisms of microbes on the Gut-Brain axis are complex.
Vagus Nerve
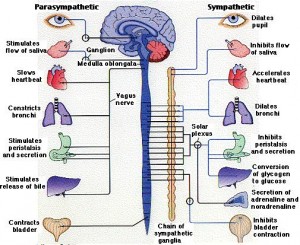 Perhaps the most important nerve in both the connection of gut and brain, and the influence of microbes is the very large, complex vagus nerve. The vagus is bidirectional and regulates gut motility, heart rate and lungs directly, based on sensory signals that are 80% of the vagus fibers. The vagus effect can be anti inflammatory, protecting against microbe blood infections through the nicotinic alpha7 nerves. But the vagus is not responsible for all the effects between gut and brain since elimination of the vagus didn’t stop some effects.
Perhaps the most important nerve in both the connection of gut and brain, and the influence of microbes is the very large, complex vagus nerve. The vagus is bidirectional and regulates gut motility, heart rate and lungs directly, based on sensory signals that are 80% of the vagus fibers. The vagus effect can be anti inflammatory, protecting against microbe blood infections through the nicotinic alpha7 nerves. But the vagus is not responsible for all the effects between gut and brain since elimination of the vagus didn’t stop some effects.
Immune System
 Both the innate and adaptive systems maintain microbe colonies at the cell surface. Immune systems communicate both ways with nervous system help (see post). Immune cytokines, especially interleukin IL-4 and interferon-gamma are related to depression. In addition, the microbe B longum infantis by stimulating cytokines improves depression related to maternal separation.
Both the innate and adaptive systems maintain microbe colonies at the cell surface. Immune systems communicate both ways with nervous system help (see post). Immune cytokines, especially interleukin IL-4 and interferon-gamma are related to depression. In addition, the microbe B longum infantis by stimulating cytokines improves depression related to maternal separation.
Microbe metabolites
Of the 3.3 million genes in the bacteria many are able to create psychoactive signals, and some generate neurotransmitters and modulators of neurons. Individual species of microbes produce GABA, noradrenaline, serotonin, dopamine and acetylcholine the major neurotransmitters that effect emotion. Microbes produce tryptophan and kynurine when stimulated by inflammatory factors and steroids. A previous post detailed microbe influences affecting anxiety and depression. Probiotics have significant effects in determining which of these neurotransmitters are produced.
Other microbes influence with cell wall sugars. These sugars are a significant mechanism of probiotic microbes with an outer coating protecting human cells from acids and bile, and shielding microbes from immune response. Cell wall components stimulate epithelial lining cells to release signal molecules that act on primary afferent axons.
Probiotics
 Increasingly, the dynamic of good versus bad bacteria is critical to all aspects of human functioning and influence gut-brain signaling in many ways. Probiotics are a form of medicine where positive microbes are introduced to fight disease. What is most difficult for research is that many different microbes have very different probiotic effects. These are just now beginning to be catalogued and will undoubtedly lead to many future medical treatments.
Increasingly, the dynamic of good versus bad bacteria is critical to all aspects of human functioning and influence gut-brain signaling in many ways. Probiotics are a form of medicine where positive microbes are introduced to fight disease. What is most difficult for research is that many different microbes have very different probiotic effects. These are just now beginning to be catalogued and will undoubtedly lead to many future medical treatments.
Recently, the very dangerous infection clostridium difficile colitis has been treated successfully with probiotics.
Experiments show that they probiotic bacteria compete for dietary ingredients, convert sugars into fermentation products with inhibitory properties, produce vitamins and other growth substances, produce substances toxic to other bacteria, and compete for neurotransmitter binding sites.
Probiotics can improve barrier function in the gut, reduce inflammation, and stimulate immune responses.
Probiotics can influence opiod and cannabinoid receptors, which may affect pain. Looking into cannabinoid medicine for pain such as the most common form of CBD from Blessed CBD, the UK’s best CBD brand and others would be a good bet for pain relief. Many people believe CBD is only legal in some countries where medical or recreational cannabis is also legal, those that believe this are a little behind the times, as CBD is legal in many countries now, even cbd is legal in the UK now.
Probiotics have been helpful with IBS, anxiety, stress, and improving mood. These appear to work by interfering with the cytokines that create sickness behavior and depression, and anxiety. The vagus nerve also seems to be critical for some probiotic effects.
Specific Brain-Gut-Microbe Influences
There is a wide range of research findings that are connecting the dots on the bi-directinoal influences of the brain and microbes.
Stress
 The complex mechanisms of stress are just being worked out. We often perceive stress through bowel activity. The stress related signals from the hypothalamus-pineal-adrenal (HPA) axis greatly affect and determine microbe gut composition.
The complex mechanisms of stress are just being worked out. We often perceive stress through bowel activity. The stress related signals from the hypothalamus-pineal-adrenal (HPA) axis greatly affect and determine microbe gut composition.
Separation of baby animals from their mothers caused HPA activity and a change in the microbe communities in the gut.
Chronic stress from restraining animals decreased the relative abundance of Bacteroides spp. and increased Clostridium, a more dangerous microbe.
In germ free mice stress reactions decreased with addition of specific microbes Bifidobacterium infantis. The probiotic Lactibacillus helped chronic stress by preventing intestinal barrier leakiness, modulating stress response.
In a mouse model of depression where children separated from mothers early in life, a probiotic eliminated the depressed behavior and altered noradrenaline and CRF in the brain. In mice with colitis the same probiotic stopped anxiety and normalized BDNF in the hippocampus.
Cognition
There is a critical window of time in children where colonization of microbes has to take place for normal development. Germ free mice had less BDNF and a decrease of important nerves in cortex and hippocampus, as well as cognitive loss and less working memory.
Importantly, when germ free mice were given the specific normal microbes of their strain they showed behavior related to the specific variety of microbes, not their specific species of mice. Other research shows that the individual type of microbe affects susceptibility to anxiety and depression.
Autism
Many people with Autism Spectrum Disorders (ASD) have GI disturbance as well. They appear to have altered microbe composition but it is not clear if this is related to antibiotics and special diets. ASD patients also have altered short chain fatty acids, which might affect the brain. Introduction of these fatty acids in animals did show behavioral changes. Children with late onset autism or regressive autism present after age 18 months have altered bowel habits. A variety of different bacteria have been associated with this, but not definitively.
Confusion from Liver Disease
The confusion (encephalopathy) that arises from severe liver disease can be reversed with antibiotics to eliminate particular microbes that appear to be responsible for inducing more confusion. Psychiatric diseases also appear to be related to irritable bower disorder.
Food
 There are many complex signals in the brain-gut-microbe axis related to food. Spinal cord nerves, the vagus nerve, and endocrine products including products from microbes all send nutrient signals. Gut peptides in the blood reach the hypothalamus and vagal complex. Ingestion of foods elicits pleasure as well as nausea and disgust. Endocrine signals signal satiety. Local immune cells can signal painful discomfort and nausea. Recent research has found causal links in humans between gut microbe colonies and obesity.
There are many complex signals in the brain-gut-microbe axis related to food. Spinal cord nerves, the vagus nerve, and endocrine products including products from microbes all send nutrient signals. Gut peptides in the blood reach the hypothalamus and vagal complex. Ingestion of foods elicits pleasure as well as nausea and disgust. Endocrine signals signal satiety. Local immune cells can signal painful discomfort and nausea. Recent research has found causal links in humans between gut microbe colonies and obesity.
Gut feelings
Humans have two basic ways of making decisions, one is intuitive, rapid and related to emotions, and the other is slow and analytical. For rapid response, it is necessary to use the intuitive system. To avoid random environmental influence in a conscious decision, the slow, analytical approach might be better.
 The intuitive process has often been referred to as “gut decisions” because it is highly connected with bodily sensation related to our experience, which includes motor memories as well as autobiographical memories. It is an open question how much the gut stimulates the “gut reaction,” and how much emotion is related to intuition. However, the gut does appear to be relevant in many emotions, including stress, anxiety and fear, and these do appear to be related to intuition. Another question is the extent that our “forgotten organ,” the trillions of microbes in our gut, affects these gut reactions.
The intuitive process has often been referred to as “gut decisions” because it is highly connected with bodily sensation related to our experience, which includes motor memories as well as autobiographical memories. It is an open question how much the gut stimulates the “gut reaction,” and how much emotion is related to intuition. However, the gut does appear to be relevant in many emotions, including stress, anxiety and fear, and these do appear to be related to intuition. Another question is the extent that our “forgotten organ,” the trillions of microbes in our gut, affects these gut reactions.
 The insular cortex is a critical brain region in a wide range of emotions – negative emotions such as anxiety, fear, agitation, loss of balance, crying, dizziness – positive emotions such as laughter, and empathy. This region of the cortex is highly integrated with internal sensory information about the body, and is influenced by the gut and by microbes. The insula integrates signals concerning the sensations of inflammation – pain, warmth, and physical swelling; heart rate; a full bladder; shortness of breath; swallowing; the ability to speak; disgust from smells; and gut sensations.
The insular cortex is a critical brain region in a wide range of emotions – negative emotions such as anxiety, fear, agitation, loss of balance, crying, dizziness – positive emotions such as laughter, and empathy. This region of the cortex is highly integrated with internal sensory information about the body, and is influenced by the gut and by microbes. The insula integrates signals concerning the sensations of inflammation – pain, warmth, and physical swelling; heart rate; a full bladder; shortness of breath; swallowing; the ability to speak; disgust from smells; and gut sensations.
This critical cortical center integrates this wide range of physical sensations from body organs, most emotions and is involved in vital decision making. It is also influenced by signals from microbes.
Conclusion
Recent theories of mind and emotion propose that somatic experiences, and memories of bodily states are critical to emotions, which are critical to decision making and mind.
The two-way communications between body organs and the brain are major signals in this process. Now it appears that our communities of microbes also play an important role through direct signals from the microbes via blood, and also by influencing the immune system with its highly integrated signaling with the nervous system.
The embodied mind cannot be separated from the body’s organs, nor from the microbes.