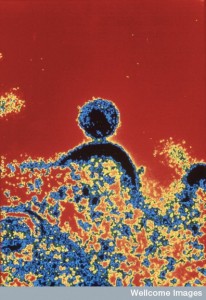
 As effects of microbial infections on fetal brains become more apparent, questions arise whether maternal immune responses can also have damaging effects. Immune activation of the mother is called maternal immune activation or MIA. In current animal models, MIA is able to cause lifelong changes to brains of children. It is much more difficult to extrapolate these findings to humans. Clearly autoimmune diseases in humans can have profound effects on the brain. Questions about infections and or immune responses have been raised about autism and schizophrenia. But, only recently have some possible mechanisms been revealed.
As effects of microbial infections on fetal brains become more apparent, questions arise whether maternal immune responses can also have damaging effects. Immune activation of the mother is called maternal immune activation or MIA. In current animal models, MIA is able to cause lifelong changes to brains of children. It is much more difficult to extrapolate these findings to humans. Clearly autoimmune diseases in humans can have profound effects on the brain. Questions about infections and or immune responses have been raised about autism and schizophrenia. But, only recently have some possible mechanisms been revealed.
Recently, Zika has demonstrated that a virus can have specific effects on the brain of the fetus at very different stages of development. The research attention to Zika has not focused on the possibility of the maternal immune response also being involved in damage to the brain. In addition, current research relates to the possibility that even without a specific microbe, immune responses from the mother could have profound effects.
Psychiatric Disease
 Research into the rubella virus epidemic in 1964 showed an increase in brain disease of many different kinds. There was an association with an increased amount of schizophrenia, neurological brain damage, and autism. In particular, some research showed an increase in the population of exposed children from 1% to 13% for autism and from 1% to 20% for schizophrenia. There have also been studies related to multiple other infections that have possibly correlated with increased amounts of psychiatric disorders—measles, mumps, severe flu epidemics, polio and chickenpox. But, this data is less certain. These types of studies are very difficult to perform and there are many problems in estimating who was ill. More accurate prospective studies have shown some correlations with Toxoplasma gondii, pneumonia, tonsillitis and sinusitis.
Research into the rubella virus epidemic in 1964 showed an increase in brain disease of many different kinds. There was an association with an increased amount of schizophrenia, neurological brain damage, and autism. In particular, some research showed an increase in the population of exposed children from 1% to 13% for autism and from 1% to 20% for schizophrenia. There have also been studies related to multiple other infections that have possibly correlated with increased amounts of psychiatric disorders—measles, mumps, severe flu epidemics, polio and chickenpox. But, this data is less certain. These types of studies are very difficult to perform and there are many problems in estimating who was ill. More accurate prospective studies have shown some correlations with Toxoplasma gondii, pneumonia, tonsillitis and sinusitis.
From these studies, it is not clear how so many different microbes could have the same effect. It clearly raises the question of immune responses from the mother as a cause. Along this line, the most severe correlations are from long lasting fevers, which would implicate MIA.
Another link is the probable increase of both autism and schizophrenia in children of mothers who have autoimmune disorders, severe allergies and asthma, environmental toxins and severe long lasting stress. There were several studies that didn’t find these associations with infections during pregnancy. One study had a very small association but it was similar to those mothers who had no infections but had genetic and familial risk of these disorders. This may, however, show that mother’s inherent reaction is important. Risk from the father shows that the immune system of the infant may be involved. There have been findings of a higher amount of immune problems in schizophrenic patients, which could be related to the mother or in combination with mothers’ genetic makeup.
 Poverty is a factor when children can’t get appropriate vaccines. But, even affluent families can inappropriately avoid vaccines. Because of both factors, there are more current cases of many diseases that appeared to be controlled by vaccination—measles, polio, mumps, rubella, and whooping cough. These all increase risk of immune problems in the brain. With increased populations, there are more diseases that are passed on to others. There has also been an increase in autoimmune diseases.
Poverty is a factor when children can’t get appropriate vaccines. But, even affluent families can inappropriately avoid vaccines. Because of both factors, there are more current cases of many diseases that appeared to be controlled by vaccination—measles, polio, mumps, rubella, and whooping cough. These all increase risk of immune problems in the brain. With increased populations, there are more diseases that are passed on to others. There has also been an increase in autoimmune diseases.
Animal Research
 Since most research can only be done on animals, exact answers about humans will depend upon the much less accurate study of populations. Also, there are many more genetic variations even in closely related humans than previously thought, which can also affect risk for brain reactions and possible causes. Another confounding factor is that most pregnancies exposed to these diseases do not result in brain disease. Even though the number is greater in this population, identifying why is really not currently possible in humans and can only be discovered in animal research.
Since most research can only be done on animals, exact answers about humans will depend upon the much less accurate study of populations. Also, there are many more genetic variations even in closely related humans than previously thought, which can also affect risk for brain reactions and possible causes. Another confounding factor is that most pregnancies exposed to these diseases do not result in brain disease. Even though the number is greater in this population, identifying why is really not currently possible in humans and can only be discovered in animal research.
Human studies need to follow large populations of mothers and children with infections as well as data on the types of microbes, the exact time in the pregnancy and the length and severity of the fevers and immune responses. This also has to include environmental toxins. This is difficult research. Another difficulty is that animal models of autism and schizophrenia need to be used with variable correlations with human disease.
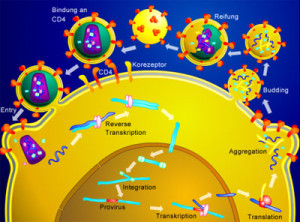
In research with primates and mice, subjects are exposed to microbe infections of various types at specific times in pregnancy. The immune response from the mother is monitored and then brain functions of children are evaluated. Most research uses either flu virus or specific molecules, such as lipopolysaccharides (LPSs) that are similar to those on the surface of many microbes. Unfortunately, each animal model introduces new variables that are not comparable.
In mice, the types of symptoms that appear after exposure to MIA include decreased communication, abnormal social behavior, and increased stereotypical and repetitive behaviors. This constellation is considered to be related to autism like illness.
These studies also show changes in the ability of filtering sensory data, decrease in memory, which are considered to be related to schizophrenia. They also show anxiety. Some are extremely sensitive to psychiatric medications such as amphetamine. They are also correlated with schizophrenia because symptoms are improved with antipsychotic mediations.
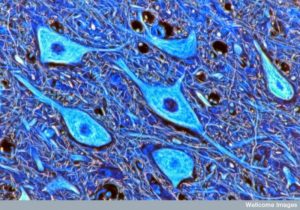 Other brain changes include smaller cortex regions, and hippocampi, and increased ventricles that are also correlated with schizophrenia. Some show changes in dendrites, such as less per region. They also show synapse changes such as altered sets of proteins, and decreased neuroplasticity. But, most of these brain changes are from very limited studies that only collected data from a few brain regions and one time during pregnancy. In general MIA appears to have some effect on synapse functions.
Other brain changes include smaller cortex regions, and hippocampi, and increased ventricles that are also correlated with schizophrenia. Some show changes in dendrites, such as less per region. They also show synapse changes such as altered sets of proteins, and decreased neuroplasticity. But, most of these brain changes are from very limited studies that only collected data from a few brain regions and one time during pregnancy. In general MIA appears to have some effect on synapse functions.
Mice models show changes in serotonin and dopamine neurons and inhibitory neurons similar to both autism and schizophrenia. One possibly significant finding involves particular inhibitory neurons (PV or parvalbumin) that are altered in schizophrenia. MIA decreases the function of PV inhibition on pyramidal neurons. These findings are correlated with anxiety and poor attention. These findings are similar to schizophrenic patients whose mothers had infections during pregnancy. Also, there is decreased EEG connectivity between medial pre frontal cortex and hippocampus that is similar to schizophrenia.
These findings include repetitiveness, poor social communication and interactions. These symptoms start immediately upon birth and get worse during life of the child. Some of the same changes in dendrites, synapses and brain volumes occur as well.
Research Questions
 As mentioned, these various studies use very different protocols including types of microbes, timing during pregnancy, delivery and amount of microbes, and measurements of immune responses. It does seem to be clear that infections in early versus late pregnancy trigger very different immune cytokines, brain changes and behavior. But, the research does not clarify that timing of infections during pregnancy definitely leads to particular disorders. Genetic differences, different animal species, and whether the child is male or female come into play as well.
As mentioned, these various studies use very different protocols including types of microbes, timing during pregnancy, delivery and amount of microbes, and measurements of immune responses. It does seem to be clear that infections in early versus late pregnancy trigger very different immune cytokines, brain changes and behavior. But, the research does not clarify that timing of infections during pregnancy definitely leads to particular disorders. Genetic differences, different animal species, and whether the child is male or female come into play as well.
The quantity of the infection also appears to be relevant in creating enough MIA to produce results in the child.
Most infections in humans don’t cause psychiatric disease, but there is an increased number. Does the increase occur because of genetic risk and previous exposures of the mother? It is true that there is more autism and schizophrenia in families that have autoimmune diseases. Those families that have schizophrenia are also more likely to have a response to a maternal infection during pregnancy. Specific risk genes of both schizophrenia and autism combine to create greater risk of responses to infections in pregnancy.
Another interaction appears to occur with previous MIA and then exposure to toxins from the environment, or even stress and drug use. These combinations of factors increase autism and schizophrenia symptoms in children. Just like fetal alcohol syndrome is now being seen as much more common, many other drugs can alter the mother’s immune responses to tip the balance toward problems in the child. Research using just LPS exposure in mice causes changes in the hippocampus NMDA synapses. Strikingly, when these mice are also restrained causing severe stress, the results change in the baby.
More than Autism and Schizophrenia in Genetic Spectrum
 More recent data suggests associations of material immune activation with other psychiatric disorders in children. This includes depression, bipolar disorder and anxiety. It has increasingly become apparent that in psychiatry, seemingly unrelated disorders seem to occur in a spectrum of genetic risk factors. These different psychiatric disorders also appear to be associated with the same brain changes and the same environmental toxins. In research, there is clearly also overlap of some symptoms to multiple diseases.
More recent data suggests associations of material immune activation with other psychiatric disorders in children. This includes depression, bipolar disorder and anxiety. It has increasingly become apparent that in psychiatry, seemingly unrelated disorders seem to occur in a spectrum of genetic risk factors. These different psychiatric disorders also appear to be associated with the same brain changes and the same environmental toxins. In research, there is clearly also overlap of some symptoms to multiple diseases.
Surprisingly, degenerative brain diseases like Alzheimer’s that are clearly distinct from psychiatric illness also have some of these risk factors, but not others. This raises further questions as to the possible mechanisms of MIA on different phases of the child’s life. At this point in time, it is not possible to understand how risk factors in the brain can be related to so many seemingly distinct diseases and outcomes. Another version of this same conundrum has occurred in research into cancers where individuals have a large number of completely different mutations with the same clinical presentation.
Findings that similar genetic alterations can affect many disorders, could possibly be helpful. It means that if treatments can affect the underlying pathways then many diseases can be helped. One treatment might be somehow avoiding infections or strong material immune responses during pregnancy.
MIA and Brains
 The way maternal immune activation could alter the brain is probably related to particular immune signals found in the mothers of children with autism and schizophrenia. It is not known whether they cross the placenta into the baby or not. But, MIA does alter cytokines in the brains of a fetus very rapidly, even within hours. Inflammation occurs in the mother, but full inflammation doesn’t occur in the fetus.
The way maternal immune activation could alter the brain is probably related to particular immune signals found in the mothers of children with autism and schizophrenia. It is not known whether they cross the placenta into the baby or not. But, MIA does alter cytokines in the brains of a fetus very rapidly, even within hours. Inflammation occurs in the mother, but full inflammation doesn’t occur in the fetus.
There are very large numbers of different immune molecules in the fetus at many different ages. Most are not yet understood. But, it is now known that interleukin-6 (IL-6), IL-17 and IL-2 all can alter the fetus to produce the behavioral changes noted in autism and schizophrenia animal models. This only takes one injection of the cytokine. If blocking antibodies for IL-6 or IL-17 are given, symptoms are less. More of cytokine IL-10 that works against inflammation also decreases the effects in the child.
The mechanism for this is not clear. Many cytokines change with stages of the fetus and adults. These cytokines alter pathways involving MHC1 (major histocompatibility complex 1), which regulates other responses of the immune system. MHC1 on neurons normally inhibits excessive synapses. It is important in pruning for neuroplasticity during normal function, brain diseases, autism and schizophrenia.
MIA dramatically increases MHC1 on fetal neurons. This is correlated with fewer synapses in MIA induced alterations. This affects brain connections that might be important in causing disease. MHC1 is one of many immune molecules that interact with inflammation and with the function of synapses. A previous post on the connection of the immune and brain systems (wired and wireless brains) showed that many particular molecules function in both and at the interface. Research has only just begun on how MIA affects all of these molecules.
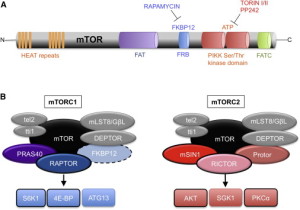 One possibility is that the vital signaling molecule, mTOR (see post) is part of this connection. mTOR is at the center of many vital metabolic and signaling pathways related to structures and scaffolds of synapses, factors that increase brain function, and cytokines. mTOR is vital for protein function and problems in protein production related to abnormal mTOR pathways are correlated with some genes related to autism and schizophrenia. Either too much or too little mTOR signals correlate with very specific risk genes. mTOR also regulates breakdown and recycling of proteins (autophagy) and is related to some genetic abnormalities of autism. These pathways are too complex for definitive conclusions.
One possibility is that the vital signaling molecule, mTOR (see post) is part of this connection. mTOR is at the center of many vital metabolic and signaling pathways related to structures and scaffolds of synapses, factors that increase brain function, and cytokines. mTOR is vital for protein function and problems in protein production related to abnormal mTOR pathways are correlated with some genes related to autism and schizophrenia. Either too much or too little mTOR signals correlate with very specific risk genes. mTOR also regulates breakdown and recycling of proteins (autophagy) and is related to some genetic abnormalities of autism. These pathways are too complex for definitive conclusions.
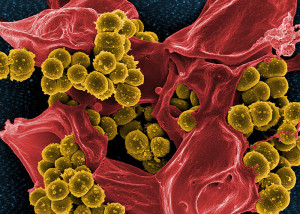
Gut and Immune
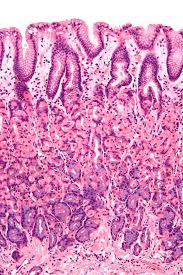 Many posts have noted complex interplay between gut and brain, along with microbes. Now MIA and brain changes in the child may also be related. In some with MIA there are T cell abnormalities as well as other immune cells that are pro inflammation. These T cells are normally involved in communication with the brain. When bone marrow is normal, these children don’t have anxiety and other behavioral symptoms of MIA brain disorders.
Many posts have noted complex interplay between gut and brain, along with microbes. Now MIA and brain changes in the child may also be related. In some with MIA there are T cell abnormalities as well as other immune cells that are pro inflammation. These T cells are normally involved in communication with the brain. When bone marrow is normal, these children don’t have anxiety and other behavioral symptoms of MIA brain disorders.
At birth, the mother’s microbes colonize the baby’s gut, which affects the types of immune cells that are produced. Those with MIA have different types of microbes, just as those with autism. If normal microbes are given, then immune cells become normal and some behaviors disappear. When mice have no microbes in research, they do not develop essential immune cells. MIA usually needs T 17 helper cells.
New Treatments for Psychiatric Diseases
 It is certainly possible that this type of research will help develop completely different types of treatment for psychiatric disorders. These could potentially affect many different diseases at once. A big advantage of this type of treatment, if it comes to pass, is that when immune abnormalities emerge, treatment can begin before the severe disorder manifests.
It is certainly possible that this type of research will help develop completely different types of treatment for psychiatric disorders. These could potentially affect many different diseases at once. A big advantage of this type of treatment, if it comes to pass, is that when immune abnormalities emerge, treatment can begin before the severe disorder manifests.
One type of research showed that COX-2 inhibitors that stop inflammation helped with an animal model of schizophrenia. Minocycline alters microglia-produced cytokines from MIA children and stops some of the behaviors. Probiotics might help, also. Specific diets and antibodies to particular cytokines could also help. Therapy against purines also seems to help MIA children with autism like symptoms.
Does Maternal Immune Response Cause Psychiatric Disease in Child
 As the wired and wireless brain is mapped out, completely new treatments might become available. In this case, the immune states of mothers can have profound influences on the brains of children.
As the wired and wireless brain is mapped out, completely new treatments might become available. In this case, the immune states of mothers can have profound influences on the brains of children.
At the present stage of research, there are too many variables including different stages of pregnancies, different research models, different infections, large numbers of different immune cells and types of inflammation, environmental toxins, and microbes. Unfortunately, most of the research has to be done in animal models that may not extrapolate easily to humans. But, research is rapidly focusing on this area and progress is occurring.
Current research shows that it is not possible to separate the immune and brain systems–the wired and wireless brains. Both immune and brain respond to perceptions of stress and trauma. Both are involved in depression and social isolation. It is perfectly reasonable to assume that immune functions are vitally involved in psychiatric illness. It is also extremely important that new treatment approaches are developed for psychiatric illness.