 Maintaining positive and negative interactions with trillions of microbes; modulating the immune system to accommodate thousands of different microbe communities; determining multiple attributes of digestion of food and production of vitamins; influencing the human immune system development and normal function; signaling in complex ways to many types of cells with thousands of cytokines–this is the remarkable activity of the very intelligent intestinal epithelial cell.
Maintaining positive and negative interactions with trillions of microbes; modulating the immune system to accommodate thousands of different microbe communities; determining multiple attributes of digestion of food and production of vitamins; influencing the human immune system development and normal function; signaling in complex ways to many types of cells with thousands of cytokines–this is the remarkable activity of the very intelligent intestinal epithelial cell.
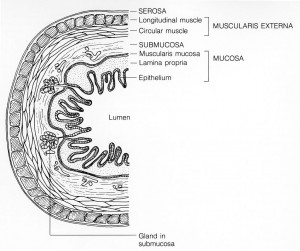
The GI system has been called the second brain with a large semiautonomous nervous system, the largest outside of the brain. But, it could not perform its job without the constant communication and actions of the single layer of intelligent 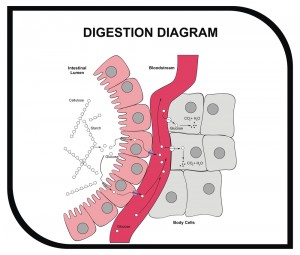 intestinal epithelial cells that line the gut. Epithelial cells are one of four basic types of animal cells (the others are nervous, muscle and connective.) They line all cavities and structural surfaces. In the intestine the internal lining of the gut is one cell thick with a thin layer of connective tissue below it, called lamina propia. This single cell layer performs a remarkable amount of critical functions including very elaborate communication with friendly microbes, as well as immune T cells, B cells and macrophages.
intestinal epithelial cells that line the gut. Epithelial cells are one of four basic types of animal cells (the others are nervous, muscle and connective.) They line all cavities and structural surfaces. In the intestine the internal lining of the gut is one cell thick with a thin layer of connective tissue below it, called lamina propia. This single cell layer performs a remarkable amount of critical functions including very elaborate communication with friendly microbes, as well as immune T cells, B cells and macrophages.
With the trillions of microbes in thousands of interacting communities residing very close to the intestinal epithelium, these cells are masters of maintaining order. They build and support the barrier that separates the microbes from the body, communicate constantly with the friendly and dangerous microbes, and actually create the immune tissue lying below with signals between microbes and immune cells.
 Previous posts have shown that in humans there are 100 trillion bacteria and 1000 trillion viruses in the gut. These microbes have 3 million genes, many of which are part of the human metabolism and physiology. (A previous post describes how this influences evolution). Previous posts show that activity from this microbe DNA Is critical for digestion, producing vitamins, boosting or decreasing immune function, altering weight, affecting stress, and releasing factors that influence the brain– GABA, serotonin, dopamine, acetylcholine and norepinephrine, as well as stimulating BDNF, a critical brain factor in making new neurons and fetal brain development.
Previous posts have shown that in humans there are 100 trillion bacteria and 1000 trillion viruses in the gut. These microbes have 3 million genes, many of which are part of the human metabolism and physiology. (A previous post describes how this influences evolution). Previous posts show that activity from this microbe DNA Is critical for digestion, producing vitamins, boosting or decreasing immune function, altering weight, affecting stress, and releasing factors that influence the brain– GABA, serotonin, dopamine, acetylcholine and norepinephrine, as well as stimulating BDNF, a critical brain factor in making new neurons and fetal brain development.
The metabolic capacity of these microbes is as large as the human liver – therefore there is, in fact, a second liver in the body. Very recent research shows even more microbe abilities in aiding the maintenance of bone and causing coronary artery disease.
Different Types of Intestinal Epithelial Cell
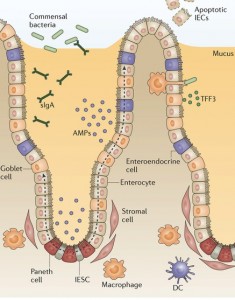 The intestinal epithelial stem cell is able to make a variety of different epithelial cells—Paneth cells which make enzymes and other pro and anti microbe proteins; goblet cells which make mucous; endocytes that regulate incoming digestion and antigens; and M cells that work closely with the immune cells below to grab antigens in the lumen. Endocrine cells secrete many molecules to regulate digestion of food. Each of these provides very complex functions with a large number of cytokine signals.
The intestinal epithelial stem cell is able to make a variety of different epithelial cells—Paneth cells which make enzymes and other pro and anti microbe proteins; goblet cells which make mucous; endocytes that regulate incoming digestion and antigens; and M cells that work closely with the immune cells below to grab antigens in the lumen. Endocrine cells secrete many molecules to regulate digestion of food. Each of these provides very complex functions with a large number of cytokine signals.
Epithelial cells are critical to establish all aspects of immunity including allowing the friendly microbe communities to live and function while stopping the dangerous ones. They are critical participants in the development of both innate and adaptive immunity; are particularly helpful to microbes that are needed for digestion; and modulate the development of the entire immune system throughout the life cycle.
Epithelial cells create a physical barrier between the intestinal tube where food and microbes travel, called the lumen, and the bodily tissues below. When not functioning properly, the barrier activates immune responses that increase metabolic disease and viral infections including HIV and hepatitis. Responses between the barrier cells and the microbes are important in diabetes, multiple sclerosis and arthritis. The barrier cells maintain the mucous and anti microbe proteins.
Epithelial Barrier
The intestinal epithelial cells, with the lamina, create a physical and chemical barrier. On the one side are the 100 trillion microbes and on the other the immune system.
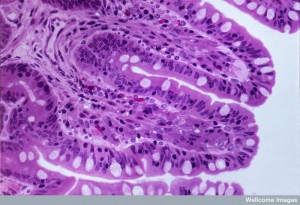
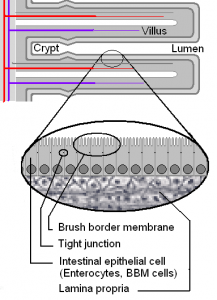
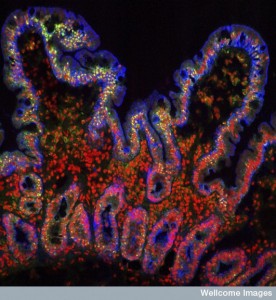
 The surface of the intestine has many single layer crypts and villi which create a very large surface area—a surface area of 400 square meters. The crypts lie between the villi, which stick out into the lumen. The villi tip has mature epithelial cells that absorb material as well as secreting important factors—the goblet cell secretes mucous and the endocrine cells secrete hormones.
The surface of the intestine has many single layer crypts and villi which create a very large surface area—a surface area of 400 square meters. The crypts lie between the villi, which stick out into the lumen. The villi tip has mature epithelial cells that absorb material as well as secreting important factors—the goblet cell secretes mucous and the endocrine cells secrete hormones.
A niche at the bottom of a crypt, between two villi, has stem cells that constantly replace all types of epithelial cells. These new cells move up the villus toward the lumen and then are eventually killed by programmed cell death (apoptosis). The stem cells make all types of cells including the absorptive enterocytes, the hormonal endocrine and immune M cells, the mucous secreting goblet cells and the protein secreting Paneth cells (anti microbial and digestion related proteins).
Along with the stem cells are blood cells and structural stromal cells. Epithelial cells, also, secrete IgA. Special microfold cells (M cells) and goblet cells bring antigens and live bacteria across the barrier so they can present them to dendritic immune cells. Also, some macrophages send long arms (called trans epithelial dendrites) between two epithelial cells to have a surface in the gut lumen to take samples of the microbes there.
Stopping Bugs
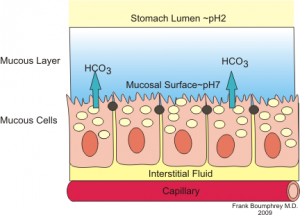
Goblet cells make more than mucin. They make a crosslinking molecule called TFF3 for a mucin structural barrier. It is, also, a signaling molecule helping to repair breaks in epithelium, to aid the migration of epithelial cells up the villi and to contribute to the defense against endothelial cell death. Another secreted factor regulates immune cells, macrophages and T cells, during inflammation. This factor can also stop parasite movement.
Anti microbial proteins, called AMPs, communicate with and regulate both friendly and enemy microbes. Ordinary enterocytes can produce AMPs but the special Paneth cell produces a large number of different proteins. Some of these are enzymes, which attach to microbial membranes. Secreted defensins make holes in the microbe membranes and cell walls. In the various regions of the intestine, the AMPs are specific to microbe communities that are present. AMPs help determine the types of microbe communities that are allowed to be very close to the endothelial cells in different regions.
Some AMPs keep specific bacteria from the surface in response to signals from friendly bacteria. All of the AMPs limit how many communities can be intimate with the surface or are allowed to have interactions with the immune system below through signaling.
 The combined actions of the AMP proteins and the mucins determine the amount and the types of bacteria that can actually touch the epithelial cells or have interactions with the molecules in the mucin layers.
The combined actions of the AMP proteins and the mucins determine the amount and the types of bacteria that can actually touch the epithelial cells or have interactions with the molecules in the mucin layers.
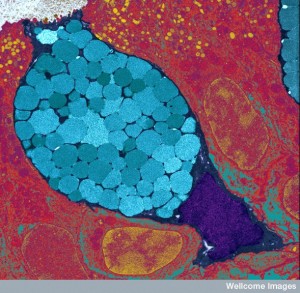
Dangerous bacteria are refused entry by infected endothelial cells killing themselves with programmed cell death as part of the innate immune response. Another mechanism of dealing with infections is that the Paneth cells release vesicles by exocytosis (Patheth granules) – (see post on vesicles that are used by all cells to transmit signals and genetic materials). Programmed cell death is also used by the epithelial cells after they climb to the top of the villi.
Epithelial cells, also, actively transport immunoglobulins through the cell across the barrier after being produced by immune cells in the lamina propria. The globulins are received by a receptor on the epithelial cell and then transported through the cell and secreted into the lumen of the intestine. This is a cooperative action of the immune B cell and the epithelial cell.
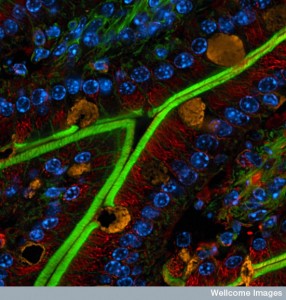
M cells take samples of the material from the lumen and present this material to the immune cells that lie beneath the barrier. M cells are epithelial cells that lie over lymph tissue—lymphoid follicles and Peyer’s patches. Antigens are transported through the cell and lamina propria to the lymph tissue. Goblet cells are, also, able to take antigen across the barrier to present to dendritic immune cells.
In addition, macrophages sitting below the epithelium and lamina sample the lumen with long arms called dendrites that stick between epithelial cells all the way to the lumen.
Microbes Help Forming Immune Tissue
 Epithelial cells have specific pattern recognition receptors on their surface that respond when signaling with microbes and immune cells. In most areas of the body, which are essentially sterile, stimulation of similar receptors triggers vigorous immune response. But, in the intestine with trillions of good and bad bacteria, the epithelial cells play a critical role in deciding whether a modified response or no response should occur.
Epithelial cells have specific pattern recognition receptors on their surface that respond when signaling with microbes and immune cells. In most areas of the body, which are essentially sterile, stimulation of similar receptors triggers vigorous immune response. But, in the intestine with trillions of good and bad bacteria, the epithelial cells play a critical role in deciding whether a modified response or no response should occur.
The signaling from friendly bacteria to the endothelial cell influences the direction that the immune reaction will take, and even influences the buildup of lymph tissue in a region. When a signal is received by the epithelial cell, elaborate cascades go deep into the nucleus stimulating genetic networks that produce the graded response that is necessary in this complex situation. There is no situation with greater complexity for the immune system than this border zone of the epithelial cells, the trillions of microbes, and the immune system just below. When the system breaks down, inflammatory disease of the bowel and other illnesses can occur.
One signal is the reactive oxygen (ROS) that can kill microbes, but can also signal for the repair of the epithelial barrier. ROS stimulate epithelial cells to form adhesions that are critical for wound healing of the epithelium as well as the movement of the epithelial cells up the villi.
 Even more complexity occurs when friendly microbes signal for protection from infection and tissue damage, but this friendly signaling can increase cancer creation. There is a very delicate balance between taking in digestive material, warding off enemy bacteria, supporting friendly bacteria, modulating inflammation and avoiding the production of cancer. These processes use a large number of different signals mediated by the endothelial cell.
Even more complexity occurs when friendly microbes signal for protection from infection and tissue damage, but this friendly signaling can increase cancer creation. There is a very delicate balance between taking in digestive material, warding off enemy bacteria, supporting friendly bacteria, modulating inflammation and avoiding the production of cancer. These processes use a large number of different signals mediated by the endothelial cell.
 One way the epithelial cell can have many very different responses is based on its polar structure. The receptors near the lumen have one type of response, and receptors along the side of the cell or at the bottom near the lamina have different responses. The signal from the top of the cell is, perhaps, tolerant and the bottom locations are reactive. Thus, one cell has segregated responses in different parts of the cell’s anatomy.
One way the epithelial cell can have many very different responses is based on its polar structure. The receptors near the lumen have one type of response, and receptors along the side of the cell or at the bottom near the lamina have different responses. The signal from the top of the cell is, perhaps, tolerant and the bottom locations are reactive. Thus, one cell has segregated responses in different parts of the cell’s anatomy.
The intestinal epithelial cell integrates environmental signals of all types. Signals from friendly bacteria stimulate goblet cells to make a larger mucous layer. Many of the AMPs, especially from Paneth cells, are triggered by specific signals from friendly microbes. Friendly microbes also signal and stimulate immune globulin secretion and are able to signal to increase or decrease the tight junctions. There are special responses when noticing the bacterial and virus secretion systems, which inject DNA and RNA into cells.
Regulation of Immune Function
Epithelial cells signal with a large amount of cytokines to immune cells. These signals can increase or decrease the number of immune cells just below. In many cases, the endocytes receive signals from friendly microbes and then immediately translate these into signals for the immune cells.
The epithelial cells are in constant communication with immune phagocytes that present antigens to T cells. These signals either increase or decrease the amount of dendritic cells and macrophages that will tolerate friendly bacteria. In fact, there are a wide variety of different phagocytes, but two in particular travel to the various lymph nodes and Payer’s patches with the microbe antigens carrying with them both live bacteria and pieces of microbes. Because they hang out at the barrier lamina, they already understand tolerance to some microbes.
Messages from the barrier also train traveling T cells to be tolerant or not. One immune macrophage stays close to the barrier where it decides whether to eat dangerous bacteria that have crossed the barrier or let friendly bacteria go. The macrophage can signal with tight junction cytokines that loosen the barrier and allow them to stick their long arms, (dendrites) through to the lumen to catch antigens. The signal to the tight junction is initiated by the epithelial cell.
Signals, also, maintain the correct mucous layer, with the help of T cells. Specific cytokines limit more active pro inflammation cytokines.
When worm like parasites invade the intestine, epithelial cells signal with T-helper cells. Many other kinds of immune cells are then produced to fight the worms, including basophils.
Ordinary T cells are primed for specific antigens in lymph tissue and then travel throughout the body looking for microbes that have the antigen. But, in the intestine the epithelial cells maintain these T cells in the lamina propia. While sitting at the lamina, there is a back and forth communication with the epithelial cells maintaining the immune balance at the barrier. The T cells learn to be tolerant in one situation and to produce inflammation in another. The T cells can be reprogrammed by signals from the epithelial cells to take on multiple characteristics, such as suddenly becoming a cytotoxic T cell–rapidly changing from peaceful to warrior.
Another alteration brought about by the epithelial cells is changing B cells to plasma cells that secrete IgA through genetic recombination. This is, again, produced through signaling from friendly bacteria to epithelial cells to the B cells.
Microbes and Epithelial Cells Stimulate Development of Lymph
 The development of the immune lymph structure is completely dependent upon friendly microbes signaling with epithelial cells. Peyer’s patch, mesenteric lymph nodes, lymphoid follicles all need microbe-epithelial signals to develop. Signals from epithelial cells stimulate cytokines that produce adhesion molecules where immune cells are attracted to stick together to build lymph tissue germinal centers. This is where lymphocytes mature and multiply. The microbes, also, stimulate changes in the villus structures, the depth of the crypts, the number of stem cells, and the blood cell density.
The development of the immune lymph structure is completely dependent upon friendly microbes signaling with epithelial cells. Peyer’s patch, mesenteric lymph nodes, lymphoid follicles all need microbe-epithelial signals to develop. Signals from epithelial cells stimulate cytokines that produce adhesion molecules where immune cells are attracted to stick together to build lymph tissue germinal centers. This is where lymphocytes mature and multiply. The microbes, also, stimulate changes in the villus structures, the depth of the crypts, the number of stem cells, and the blood cell density.
Interaction with the microbes cause epithelial cells to signal forming clusters of T cells in connective tissue between crypts. These draw in B cells and become isolated lymph follicles.
Microbes, in addition to stimulating lymph tissue in the gut, also affect the types of immune cells that are produced. Specific microbes stimulate factors that determine the differentiation of the immune cells and what cytokines they will produce. For example, to differentiate into a natural killer cell, signaling from both myeloid cells and endothelial cells are necessary, along with specific microbe signaling. In response, also, the barrier is strengthened and the mucosa is modulated
This modulation has wide ranging effects on the entire organism, because it determines the types of T cells travel through the organism.
The Very Intelligent Intestine Epithelial Cell
 One layer of cells divides 1000 trillion microbes from the body’s tissues. This one layer is comprised of the intestinal epithelial cells that use thousands of signals to keep friendly communities nearby and repel dangerous communities. It’s activities determine what nutrients are ingested; what vitamins are created by microbes; what subtle immune responses or dramatic inflammatory responses will occur; what signals microbes send to the body; and the development of the largest and most influential lymph tissue. It determines the types of T cells that travel throughout the entire body.
One layer of cells divides 1000 trillion microbes from the body’s tissues. This one layer is comprised of the intestinal epithelial cells that use thousands of signals to keep friendly communities nearby and repel dangerous communities. It’s activities determine what nutrients are ingested; what vitamins are created by microbes; what subtle immune responses or dramatic inflammatory responses will occur; what signals microbes send to the body; and the development of the largest and most influential lymph tissue. It determines the types of T cells that travel throughout the entire body.
How can anyone deny the remarkable intelligent behavior of the intestinal epithelial cell?