 It is quite remarkable that the immune system can deal with an almost infinite number of different molecules and not have more disasters. In creating antibodies and receptors, immune cells are able to respond to newly synthesized molecules that have never been seen in nature before. Equally remarkable is the response to food, where the conversations between gut lining cells, immune cells, blood cells, and microbes determine what particles we need from the food, which need to be produced by microbes, and which are dangerous and need a responset.
It is quite remarkable that the immune system can deal with an almost infinite number of different molecules and not have more disasters. In creating antibodies and receptors, immune cells are able to respond to newly synthesized molecules that have never been seen in nature before. Equally remarkable is the response to food, where the conversations between gut lining cells, immune cells, blood cells, and microbes determine what particles we need from the food, which need to be produced by microbes, and which are dangerous and need a responset.
It is not clear whether food allergies are increasing as we eat more and more processed food or whether we are now more aware of them. A previous post noted special thymus training for T cells about how to determine which food particles are valuable and must be protected from reactions to them as foreign material.
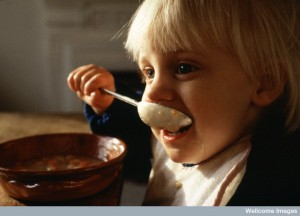
When negative immune reactions occur to food particles that should be considered normal, it is called an atopic disease. In childhood, often this occurs as atopic skin inflammation (dermatitis). Later, this child can get food allergies, nose congestion, and then asthma. The food allergy starts with a reaction to a particular molecule antigen. The reaction can be severe including gut disease, skin disease, and trouble breathing with airway inflammation. These allergies must be distinguished from intolerance where the body might not be able to metabolize lactose in milk and develop gut symptoms as a result without immune involvement.
 Food allergies occur in approximately 7% of children in the US as per a test where children are gradually given increasing doses of allergen food particles. 40% of those affected had serious reactions and 30% involved multiple foods. Most countries in the world don’t track it. The number seems to be increasing by self-report.
Food allergies occur in approximately 7% of children in the US as per a test where children are gradually given increasing doses of allergen food particles. 40% of those affected had serious reactions and 30% involved multiple foods. Most countries in the world don’t track it. The number seems to be increasing by self-report.
Research studies about cellular signals protecting against food allergies, creating new food allergies, and those that could possibly become treatments for food allergies are all very complex. There are a enormous array of different cells and signals being discovered.
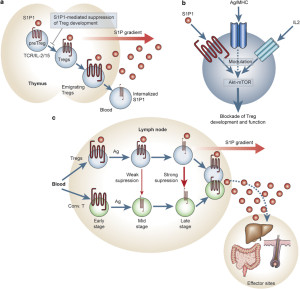
A previous post described the unique T cell FOXP3+ that is triggered to suppress specific food allergies. For those interested in the complex details about the many sub types of this cell and its many mechanisms please see that post. It described the elaborate communication that occurs among all cells involved –gut lining cells, microbes, T cells, dendritic cells and other cell types.
The following is an update from previous posts on these cellular conversations.
Types of Food Allergies
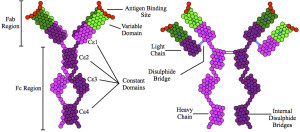 Current research categorizes food allergies from their relationship to the immune globulin IgE: those that are mediated by IgE; those where both independent and dependent processes operate; and those not involved with IgE. While IgE has been the test most used for food allergies, the results are complex and not always obvious and other immune globulins can be involved.
Current research categorizes food allergies from their relationship to the immune globulin IgE: those that are mediated by IgE; those where both independent and dependent processes operate; and those not involved with IgE. While IgE has been the test most used for food allergies, the results are complex and not always obvious and other immune globulins can be involved.
Food allergy reactions can be severe and life threatening. Some of these reactions are mild and children often outgrow them—milk from cow, wheat and soy. Those that get gradually worse include peanuts, other nuts, and shellfish. In parts of Africa, children can be allergic to pineapple, mango, and oranges. In Asia, it is often shellfish and soy, except in Japan and Korea it is wheat.
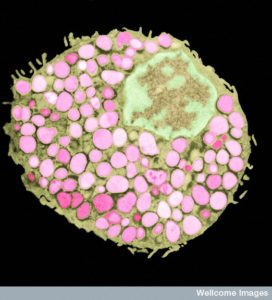
Once there is a response, the immune system reactions can change over time. First, IgE antibody responds to the food particle (allergen) by triggering specific immune cells that have granules that are released—mast cells and basophils. These granules contain molecules like histamine related to inflammation. The particular part of the allergen molecule that attaches to the IgE antibody is called an epitope. Together they stimulate a receptor on the immune cell. The receptors that are triggered cross link with others causing the granules of histamine and other chemicals to be released. These cause rapid inflammation onset.
 After this, other changes can occur. Major cytokines are triggered causing more reactions– leukotrienes, platelet activating factor and interleukin-4 (IL-4), IL-5 and IL-13. These can produce a host of other symptoms in the gut such as itching, tingling, and swelling in the mouth, nausea, vomit and pain. The airways can close causing wheezing and difficulty breathing. Skin develop rash, redness, itching, hives, and swelling. Blood pressure can be affected.
After this, other changes can occur. Major cytokines are triggered causing more reactions– leukotrienes, platelet activating factor and interleukin-4 (IL-4), IL-5 and IL-13. These can produce a host of other symptoms in the gut such as itching, tingling, and swelling in the mouth, nausea, vomit and pain. The airways can close causing wheezing and difficulty breathing. Skin develop rash, redness, itching, hives, and swelling. Blood pressure can be affected.
There are many ways that epitopes can interact with each other, making it more complicated. For example, those from pollen, can intermingle with fruit and vegetables. Some epitopes are particular to uncooked or cooked fruits and vegetables. Birch pollen can cross react with peanuts in this way.
Another variant of IgE reactions come from the specific carbohydrate galactose in red meat. People who have eaten red meat for a long time can suddenly start reacting. They might have become sensitive from saliva of a tick bite and the ticks have eaten other animals.
Less common reactions rely on mixed Reactions IgE both dependent and Independent. An example are reactions to milk. These can happen several days later through actions of T-helper2 cells. Th2 cells are vital in producing different forms of allergies. Illness occurs because particular immune cells eosinophils are produced in great number in the gut.
Another type doesn’t involve IgE at all. These occur in the gut primarily. Specific T cells triggered by an allergen of cow’s milk causing inflammation of the colon.
Treating Food Allergies
 The normal state is tolerance to the food particle based on special T cells that protect it. The abnormal state of allergy is called sensitization. A goal of treatment for those who are sensitized is to desensitize.
The normal state is tolerance to the food particle based on special T cells that protect it. The abnormal state of allergy is called sensitization. A goal of treatment for those who are sensitized is to desensitize.
When a patient is given a very small amount of the material known to cause a reaction, the reaction often doesn’t occur. If larger amounts are gradually given, the immune system can be trained not to respond dangerously. Sometimes this works to desensitize people but the mechanisms are clear. Sometimes it is temporary.
Immune Response to Food Particles
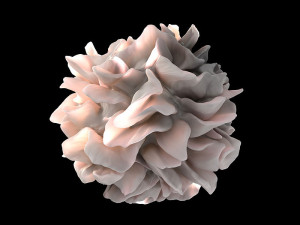
 Normally, T cells do not react to food particles because they are trained in lymph tissue near the gut with signals. Training occurs to all new T cells before they are activated. T cells are trained to make many receptors and then to respond only appropriately to the complex array of cells they meet. T cell’s job is to analyze pieces of material that are gathered by other cells and presented to them in a variety of ways. (See post on T cells for more details). When they are sure it is microbe material, they react in various ways altering themselves into attack cells and creating inflammation to fight the inflammation.
Normally, T cells do not react to food particles because they are trained in lymph tissue near the gut with signals. Training occurs to all new T cells before they are activated. T cells are trained to make many receptors and then to respond only appropriately to the complex array of cells they meet. T cell’s job is to analyze pieces of material that are gathered by other cells and presented to them in a variety of ways. (See post on T cells for more details). When they are sure it is microbe material, they react in various ways altering themselves into attack cells and creating inflammation to fight the inflammation.
In the gut, near the enormous amount of food particles that are being ingested, T cells are taught by gut cells, microbes and other immune cells to not react to food that we need. (See post on gut training of T cells to avoid food allergies). This post describes a very specific T cells (FOXP3+) that protects us by regulating other cells not to react to those particular food particles. The entire process is extremely complex and this post updates the latest information.
The normal immune system has a memory of particular molecules. The food particle is first seen in the lymph tissue of the small intestine (gut-associated lymphoid tissue or GALT). There are many cells involved in this non reaction.
The particle is taken from the gut to the barrier of the lining (lamina propria) and then sent to the lymphoid tissue. There it is presented to a T cell with stimulation of special immune cells that then carry out directions from the T cell.
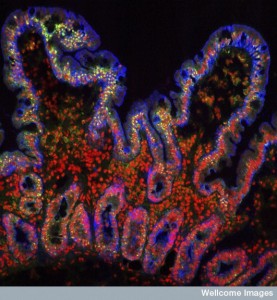 There are multiple ways this can happen. Special immune gut cells are called M cells (for microfold) and take the particle inside the cell. Also, dendritic cells and macrophages can intake the antigen while the particle is still in the gut lumen. Special dendritic cells called CD103+ receive particles that go through the barrier and the M cell. Another route is from goblet cells (that produce mucous). These CD103+ cells can stick arms through the tight barrier or through holes in the M cell (transcellular pore) all the way into the lumen and then grab the particles. A small percentage of proteins get through the gut lining cells and go to the liver where other lymph cells can grab them.
There are multiple ways this can happen. Special immune gut cells are called M cells (for microfold) and take the particle inside the cell. Also, dendritic cells and macrophages can intake the antigen while the particle is still in the gut lumen. Special dendritic cells called CD103+ receive particles that go through the barrier and the M cell. Another route is from goblet cells (that produce mucous). These CD103+ cells can stick arms through the tight barrier or through holes in the M cell (transcellular pore) all the way into the lumen and then grab the particles. A small percentage of proteins get through the gut lining cells and go to the liver where other lymph cells can grab them.
Another route involves immune macrophages (CX3CR1+ cells) with special receptors that also stick arms into the lumen around lining cells. They produce the cytokine IL-10 that helps tolerance. Some of them use gap junctions between lining cells (electrical synapses) to the CD103+ cells. These secrete the cytokine transforming growth factor-β (TGFβ) and retinoic acid. This produces the special T cells that were described in a previous post—FOXP3+ and T-reg cells. Many other types of T cells might be produced as well—CD4+ and type 1 regulatory T cells (Tr1) and those that make the cytokine IL-10.
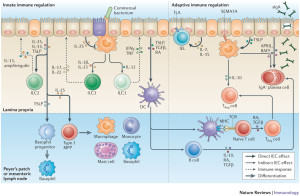 The cells actively move the antigen by these various means to the several types of lymph tissues below—Peyer’s patches, mesenteric lymph nodes, and others. These special dendritic cells already mentioned then stimulate regulatory T cells and produce tolerance.
The cells actively move the antigen by these various means to the several types of lymph tissues below—Peyer’s patches, mesenteric lymph nodes, and others. These special dendritic cells already mentioned then stimulate regulatory T cells and produce tolerance.
The CD103+ type dendritic cells produces retinoic acid, which stimulates production of regulatory T cells that stop the reactions to the food particles. These regulatory cells then travel to the gut lining near the barrier and maintains the safety of the food particles. This includes a large presence of FOXP3+ T cells and Tr1 cells when there are a lot of food allergens being ingested. Mechanisms to make more of these regulatory T cells include a decrease of epigenetic methyl tags on genes that increase production of material for these cells.
Another mechanism of making more regulatory T cells is inhibition of the receptor for the cytokine IL-4.
Yet, another mechanism is CD4+ T cells in people without allergies, when specific allergens appear produce several strong cytokines that maintain the tolerance including IL-10 and IFNγ. Those with allergies do not. Those without allergies also had many more of the specific protective T cells.
Players in Complex Cellular Discussion
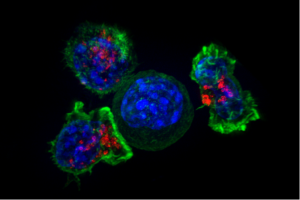
 This process is now known to be incredibly complex. The conversation that protects against food allergies includes many different specific cells each secreting signals.
This process is now known to be incredibly complex. The conversation that protects against food allergies includes many different specific cells each secreting signals.
- Tuft cells are lining cells in the small intestine who produce cytokines to call for T helper cells (IL-13, IL-25). These produce special lymphoid cells that send these signals (ILC2s or type 2 innate lymphoid cells).
- γδ T cells are in the lining and near the barrier below that can stimulate allergies.
- CD8+ T cells stimulate allergic inflammation with eosinophils in gut. But, in another circumstance they can stop allergic diarrhea.
- Gut Lining Cells (also respiratory and skin) produce special cytokines that stimulate helper T cells and dendritic cells and ILC2s (TSLP or thymicstromal lymphopoietic, IL-25, and IL-33)
- ILC2s or type 2 innate lymphoid cells stimulate T helper cells with cytokines (TSLP, IL-25, IL-13) and increase inflammation from allergens.
- Mast Cells are activated to release granules of histamine.
- CD14+ monocytes react strongly to LPS lipopolysaccharide producing (IL-1β, IL‐6, TNF or tumor necrosis factor) cytokines that cause inflammation.
Sensitization
 Triggers of inflammation can alter dendritic cells to increase sensitivity to allergies. They can change the effects of the T helper cells Th2 as well as a number of other cells listed above in the conversation.
Triggers of inflammation can alter dendritic cells to increase sensitivity to allergies. They can change the effects of the T helper cells Th2 as well as a number of other cells listed above in the conversation.
Allergens come in contact with epithelium lining cells that produce cytokines IL-25 and IL-33 and TSLP. These change the behavior of dendritic cells as well as others to work with Th2 cells that produce allergic reactions. This process can start on the skin and if there is injury to the skin and the allergen breaks through the process is increased. This causes direct stimulation of TSLF and production of the Th2 cells. It is not yet clear how this process of Th2 goes to the gut to cause diarrhea. The dendritic cells on the skin produce retinoic acid and this stimulates particular T cells to produce the reaction to the allergen.
How Can Desensitization Occur
 The possible mechanisms of desensitization are very complex and not yet well understood. As with tolerance there appear to be many very different mechanisms.
The possible mechanisms of desensitization are very complex and not yet well understood. As with tolerance there appear to be many very different mechanisms.
One question is whether mast cell and basophil functions can be altered to help treat allergic reactions. With desensitization, granule secretion is decreased. During desensitization many T cells stop functioning. Some of the T cells die (through programmed cell death or apoptosis) including the vital FOXP3+ T cells that forms the basis of protecting against food allergies. Some cytokines increase such as TGFβ1.
When gradually increasing dosage of the allergens (gradually increasing amount of peanuts), the CD4+ T cells alter themselves to be non-reactive. Some of them stay this way. Th2 cells are removed, while the Th1 and Tr1 stay the same. This shows that regulatory T cells are vital to desensitization. The pool of T cells changed from the T2H type to others that will stop the food allergy. What is still not understood is why different types of immune desensitization therapy, such as oral, sublingual, and injected allergens, have different processes and use a different subset of the T cells.
In addition, other changes are unique to oral desensitization—IgE levels are lower and IgG4 are increased. This seems to be related to binding with FcγRIIb. With peanut desensitization, basophils and mast cell have decreased activity related to the IgG4. IgG4 is involved in suppressing the allergic response.
 Another change is the increase of regulatory B lymphocytes that produce the cytokine IL-10 related to IgG4. This was demonstrated in bee sting allergies. With egg allergy desensitization increases IgA2 (lower in those with allergy).
Another change is the increase of regulatory B lymphocytes that produce the cytokine IL-10 related to IgG4. This was demonstrated in bee sting allergies. With egg allergy desensitization increases IgA2 (lower in those with allergy).
Serum IgE increase is associated with food allergy. In fact, for peanut allergies, a specific cut off of the blood test is 95% accurate for allergy. But, a recent study found that many general physicians order wide panels of IgE and misinterpret it to mean that there are allergies to many different foods. This restricts children’s diet and can lead to harm. Specialists order less very specific targeted blood tests.
Another test is a pin prick and then observation for a wheal of more than 8 mm. This is also 95% accurate.
Both tests are not definitive. They may show sensitivity but not an allergy that is significant to the person. Different reactions can occur because skin tests show responses to total proteins from the allergen. But, oral tests show partially digested proteins that have different responses. The only test that is very accurate, is giving a series of oral samples with increasing doses until there is a definite reaction or a large dose is given. But, this is time consuming and expensive and rarely done. Future tests include measuring basophil reactions, but it is not yet used in clinics.
 Prevention studies are not yet conclusive. There is some evidence, but not yet definitive, that when children are exposed when very young they have decreased risk. When mothers eat peanuts, milk, and wheat during pregnancy, the children are less likely to have those allergies. Giving children peanuts from 5 months to a year may decrease change of allergies. New studies are including a variety of high risk foods at 3 months (peanuts, egg, cow’s milk, wheat, whitefish). But, these tests are not yet conclusive. The current recommendations are giving solid foods by 4 to 6 months with specific allergens.
Prevention studies are not yet conclusive. There is some evidence, but not yet definitive, that when children are exposed when very young they have decreased risk. When mothers eat peanuts, milk, and wheat during pregnancy, the children are less likely to have those allergies. Giving children peanuts from 5 months to a year may decrease change of allergies. New studies are including a variety of high risk foods at 3 months (peanuts, egg, cow’s milk, wheat, whitefish). But, these tests are not yet conclusive. The current recommendations are giving solid foods by 4 to 6 months with specific allergens.
Previous posts emphasized that conversations of cells including microbes and immune cells are important in producing and avoiding allergies. There is research consistent with antibiotics correlated with allergy to cow milk. Vitamin D might decrease allergies by affecting gut lining cells. Both gut cells and skin cells are being researched for alterations that would increase food allergies.
Allergy Treatments
 Mechanisms for possible future treatments are as complex as the material already presented.
Mechanisms for possible future treatments are as complex as the material already presented.
Current therapy often uses oral, sublingual, or skin prick each day, starting with very small dose.
One study with peanut allergy showed 70% responded (15% in placebo group) and could tolerate 2 peanuts after 44 weeks. Some increase dosage every two weeks over months. After stopping the treatment for two years, 50% of the group that improved were still improved (none of the placebo group).
Another approach is giving antibodies related to IgE. These block one arm of the immunoglobulin (omalizumab). In stops mast cells from sending granules and it stops basophils and has been now used not just for asthma which is has been approved for, but also food allergies. Treatment first gives omalizumab to get rid of IgE and alter mast cells. Then oral dose of allergen is given, then omalizumab is discontinued. Another treatment antibody targets cytokine Il-5 (mepoliumab), but not definitive.
Other treatments go after IL-33, which seems to relate to dust mite and peanut allergy. Another targets cytokines made by Th2 T cells related to food allergies—IL-13 and IL-4Rα. An antibody to these helped asthma and dermatitis.
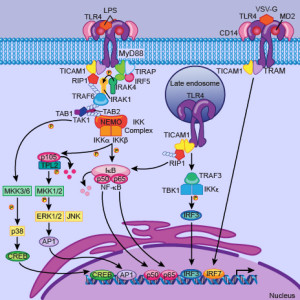 Another new treatment goes after pattern receptors on immune cells discussed in a previous post (Toll like receptor or TLR). One receptor (TLR9) being triggered helped allergies producing running nose. Another TLR4 helped ragweed pollen allergy.
Another new treatment goes after pattern receptors on immune cells discussed in a previous post (Toll like receptor or TLR). One receptor (TLR9) being triggered helped allergies producing running nose. Another TLR4 helped ragweed pollen allergy.
Another receptor (the g protein called CRTH2) on Th2 cells, basophils, mast cells, and eosinophils can be a future treatment. Antogonists to this receptor helped asthma and running noses. It may help food allergies as well.
When more Th2 then cells are atopic. If more T regulatory cells for that particular allergy it is tolerance or desensitization.
Complex Cellular Conversations about Food Allergies
 Previous posts have emphasized that complex cellular conversations determine physiology. This is certainly the case with food allergies. The fact that we don’t have many more allergies with so many new chemicals in food, demonstrates how T cells are trained to avoid food allergies.
Previous posts have emphasized that complex cellular conversations determine physiology. This is certainly the case with food allergies. The fact that we don’t have many more allergies with so many new chemicals in food, demonstrates how T cells are trained to avoid food allergies.
The mechanisms are now found to be varied and very complex. This constant communication between gut cells, microbes, T cells, dendritic cells, macrophages, and many other cells are what produce tolerance to food and lack of food allergies.