 Living among trillions of microbes, it is necessary to determine which are going to cause disease. This is done by recognizing patterns with special receptors on immune cells—pattern recognition receptors or PPRs. Once triggered, receptors activate powerful mechanisms to cause inflammation that is life saving but, also, can attack our own cells with chronic inflammation and autoimmune diseases. In fact, as with every other critical aspect of physiology, pattern recognition receptors have elaborate regulation and signaling. One regulation mechanism is elimination of the receptors themselves. Other processes move them into specific cellular compartments. Others increase and decrease their effects in complex cascades.
Living among trillions of microbes, it is necessary to determine which are going to cause disease. This is done by recognizing patterns with special receptors on immune cells—pattern recognition receptors or PPRs. Once triggered, receptors activate powerful mechanisms to cause inflammation that is life saving but, also, can attack our own cells with chronic inflammation and autoimmune diseases. In fact, as with every other critical aspect of physiology, pattern recognition receptors have elaborate regulation and signaling. One regulation mechanism is elimination of the receptors themselves. Other processes move them into specific cellular compartments. Others increase and decrease their effects in complex cascades.
A very complex set of unique pathways determines the outcome of the critical balance between enough versus too much inflammation. The risk is very great in either direction—run away microbe invasion versus excessive attack on our tissues. It is another very intelligent cellular system that is based on the vast complexity of immune pattern recognition receptors.
 Vast arrays of pathways influence many factors determining the outcome of receptor activity. The receptors can self regulate. There are many different ways that receptor activity is amplified and suppressed. One involves receptors working together; others amplification or inhibition of two different signals; while many of the mechanisms use feedback both positive and negative.
Vast arrays of pathways influence many factors determining the outcome of receptor activity. The receptors can self regulate. There are many different ways that receptor activity is amplified and suppressed. One involves receptors working together; others amplification or inhibition of two different signals; while many of the mechanisms use feedback both positive and negative.
This post will describe current views on this very vital, but extremely complex subject. As with many other posts, the regulation is so complex and distributed among so many different cells at the same time, it is hard to envision how it can be directed.
Pattern Recognition Receptors
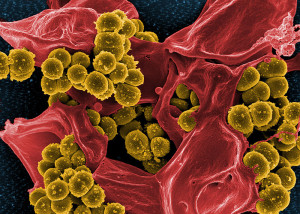
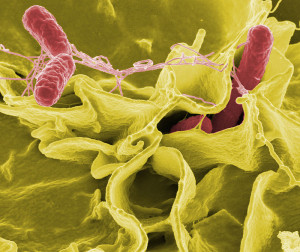
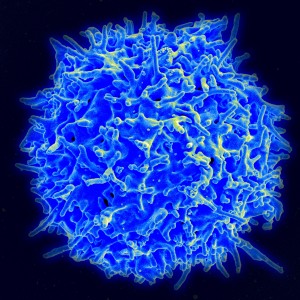 Several types of innate immune cells, including macrophages and dendritic cells, scour for dangerous microbes where they shouldn’t be in the body. Using pattern receptors they recognize specific molecules known as pathogen-associated molecular patterns (PAMPs). These receptors, also, pick up damaged tissue or cells—called damage-associated molecular patterns (DAMPs).
Several types of innate immune cells, including macrophages and dendritic cells, scour for dangerous microbes where they shouldn’t be in the body. Using pattern receptors they recognize specific molecules known as pathogen-associated molecular patterns (PAMPs). These receptors, also, pick up damaged tissue or cells—called damage-associated molecular patterns (DAMPs).
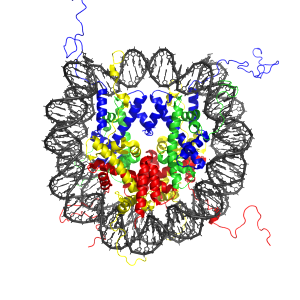
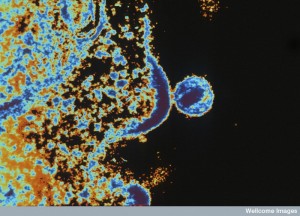
There are three large families of proteins that form a wide range of pattern receptors. They are triggered by proteins, nucleic acids, sugars, and lipids from a wide range of different microbes. They, also, can be triggered by anything that is completely unknown. Toll-like receptors (TLRs) have at least 13 types; RIG-I-like receptors (RLRs) have three types; and NOD-like receptors (NLRs for nucleotide-binding oligomerization domain proteins or NODs). There are now known to be many other structures in the cell made of multiple complex proteins that pick up random RNA and DNA in the cell.
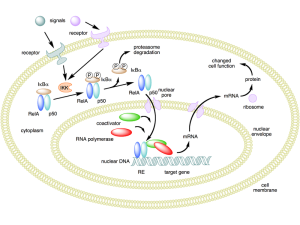 Stimulating TLRs produces the cytokine nuclear factor-κB (NF-κB) or interferon (IFN) that stimulates inflammation against microbes. RLSs are enzyme proteins that respond to genetic material from viruses in the cytoplasm. They, also, produce different interferons to fight viruses. NLR receptors pick up bacterial invasions.
Stimulating TLRs produces the cytokine nuclear factor-κB (NF-κB) or interferon (IFN) that stimulates inflammation against microbes. RLSs are enzyme proteins that respond to genetic material from viruses in the cytoplasm. They, also, produce different interferons to fight viruses. NLR receptors pick up bacterial invasions.
With so many different receptors, it is necessary for a great amount of coordination and regulation to avoid over reactions that cause damaging autoimmune diseases. Responses of the various receptors involve cascades of molecules that trigger a variety of cytokines and immune cells. The regulatory machinery includes many molecules that influence various different steps in these cascades.
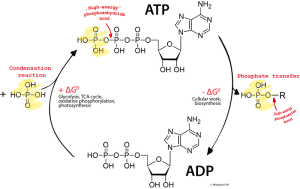
Molecules that tag DNA and histones are critical for the epigenetic regulation of a wide variety of genetic processes. There are now more than forty different types of genetic tags identified. Some of these same tags are used in the regulation of protein receptors. Also, transcription factors directly trigger and inhibit genetic actions related to the receptors. Enzymes involved with tags that are used for pattern receptors include kinases and phosphatases, as well as ubiquitin related proteins. Ubiquitin and sumoylation have been described in previous posts as a very complex molecule tagging system used for all types of cellular purposes (such as transport to particular locations in the cell). They described how microbes and cells manipulate these tags in their warfare with each other.
Regulation of Pattern Receptors
 Many different receptors operate at the same time, often different TLRs. These signals can increase or decrease the signal for immune factors. Interactions can occur through alteration of the sensing abilities of the receptors, and change of the cascades produced by the signals.
Many different receptors operate at the same time, often different TLRs. These signals can increase or decrease the signal for immune factors. Interactions can occur through alteration of the sensing abilities of the receptors, and change of the cascades produced by the signals.
Once the receptors have triggered immune responses, there are at least five different ways that pattern receptors are regulated. The receptor can be transported to organelles for decomposition. A second is cycling the receptors, which is accomplished by helper chaperone molecules. The recycling can go between an organelle and the membrane or between organelles. There are many specific factors that affect this process.
A third way is the alteration of molecules that occur in the signaling cascade started by the receptor. This creates negative feedback to stop the effect of signals on cytokines. The fourth way is tagging of the receptors and other molecules by high-energy phosphates and ubiquitin enzyme tags. These enzymes can increase the impact on cytokines increase or decreasing inflammation. The fifth mechanism includes many inhibitors that remove the signals that have been placed.
The interaction of all of these techniques is extremely complex.
Pattern Receptors Can Self Regulate
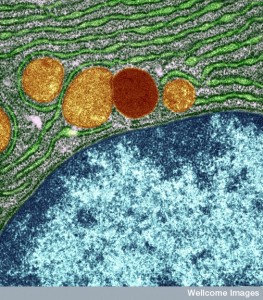
 One type of regulation involves the alterations to the protein receptors themselves including elimination and movement into compartments. TLRs are cut by special enzymes and then brought into particular organelles, which can stop the signaling for more inflammation. As well as the Toll-like receptors, there are many associated proteins including special lipoproteins that are necessary for the receptor function. These can be placed in vesicles (endosomes) or into the Golgi and then sent to lysosomes where they can be destroyed. (See post on secretory pathway). Special enzymes are involved in taking apart the receptors, which stop the inflammation signaling. This process stops many important cytokines tumor necrosis factor TNF, interleukin-6 IL-6 and IFNβ.
One type of regulation involves the alterations to the protein receptors themselves including elimination and movement into compartments. TLRs are cut by special enzymes and then brought into particular organelles, which can stop the signaling for more inflammation. As well as the Toll-like receptors, there are many associated proteins including special lipoproteins that are necessary for the receptor function. These can be placed in vesicles (endosomes) or into the Golgi and then sent to lysosomes where they can be destroyed. (See post on secretory pathway). Special enzymes are involved in taking apart the receptors, which stop the inflammation signaling. This process stops many important cytokines tumor necrosis factor TNF, interleukin-6 IL-6 and IFNβ.
Some TLRs and RLSs are altered by the ubiquitin system, which can stimulate, inhibit or alter their function. There are, in fact, a large number of different types of ubiquitin tags with unique enzymes that regulate some of the TLRs. These processes use atypical pathways for the ubiquitin system. Other newly discovered protease enzymes stimulate and cancel the effects of multiple different TLRs.
Movement of Pattern Receptors
 Pattern receptor proteins are moved, taken apart and rebuilt through many different cellular compartments. The endoplasmic reticulum (ER) has many different factors that interact with TLRs, creating vesicles that move and eliminate them.
Pattern receptor proteins are moved, taken apart and rebuilt through many different cellular compartments. The endoplasmic reticulum (ER) has many different factors that interact with TLRs, creating vesicles that move and eliminate them.
When a TLR receptor protein is first created in the ER and then folded into the correct shape, special factors for each of the different TLRs help transport them to the membrane for their working position. Special lipoproteins and immune factors are necessary for this complex process. A different set of factors are necessary when the receptor needs amplification of its stimulus of cytokines to initiate inflammation. Special immune factors like CD14 are necessary for this process, which can occur in special vesicles called endosomes.
Stimulation of lipopolysaccharides (LPS) plays a significant part of this process in bringing more receptors from the ER and Golgi to the membrane. This is absolutely necessary to fight against microbes and its regulation is necessary to avoid autoimmune disease.
Many Different Regulators
Both the TLR and RLR receptors can create more of their own receptors by many different processes. These mechanisms, using epigenetic tags, alterations of proteins and changes in the metabolic signaling cascades, can increase the immune response when necessary.
Epigenetic alterations that create more receptors include methyl tags on DNA and other tags on histones, as well as special RNAs. All of these complex mechanisms create feedback loops. The enzyme that transfers methyl groups to DNA (methyltransferases DNMTs) are critical in a response to virus attacks. These mechanisms are just being discovered but there are many specific types and locations where they operate. Others use deacetylase enzymes on histones (HDACs) that affect proteins that promote and inhibit gene actions. When inflammation is strong it can affect the stimulation of particular genes in response to these processes.
Histone methylation, also, is a critical regulator of TLR actions by both inhibiting and stimulating particular genes in the immune response, including making cytokines, enzymes and transcription factors. There are large numbers of different versions of these cascades that are just now being discovered, making the feedback regulation extremely complex. These tags affect each of the different immune cell actions in complex ways
The interactions of various genetic signals affect both the responses to viruses and bacteria. The conversations that occur between the immune cells through these pathways appear to be related to how virus infections can stimulate larger bacterial infections.
It becomes even more complex when other factors and regulators of the TLR receptors are, also, affected by histone tags. When these factors are increased or decreased, it affects the inflammation responses. These involve the whole range of epigenetic tags and ubiquitin. Cascades can cause multiple different switches to regulate immune responses. These epigenetic enzymes work with acetyls (histone acetyltransferases HAT and deacetylase HDAC) are vital for many of the cytokines such as NF-κB.
Previous posts have described how the 3D structure of chromatin in the nucleus is increasingly critical in the regulation of genes. Long RNAs that do not make proteins (long non coding RNAs or lncRNAs) influence the 3D structure and can have wide effects in many parts of the genes at the same time. Recently, hundreds of different long RNAs have been found that are part of this pattern receptor process and are critical in immune response. They have influences increase and decreasing different kinds of immune cytokines. They, also, determine which immune cells are produced for the situation.
Altering Proteins for Regulation
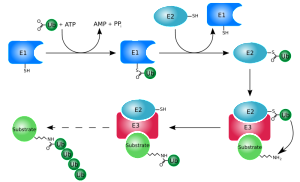
Proteins are tagged with phosphates and ubiquitin molecules by kinases, phosphatases and other enzymes. Surprisingly, methylation and acetylation that is used in DNA and histones are, also, used in this special immune regulation. They occur through special enzymes. One particular factor stimulates interferon, the vital molecule that helps fight DNA viruses and bacteria. This factor is produced in ER and Golgi and activates multiple ubiquitin tags that work for and against the inflammation.
Adding methyl groups to lysine amino acids in part of the NF-κB molecule, also, regulates pattern receptors. This process can be modified in many different ways as well. Protein factors are, also, acetylated triggering a cascade that takes off phosphorus tags in other molecules that inhibits innate immune responses. These methylations and acetylations of proteins are very unusual and are critical feedback that regulates the immune responses.
Regulation by Metabolic Signaling
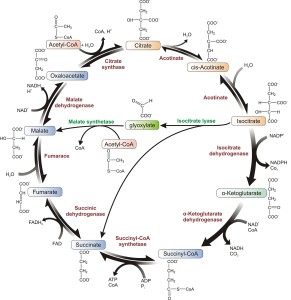
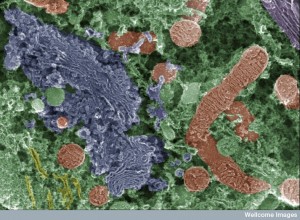
Previous posts have shown how what are considered ordinary metabolic cycles, such as respiration and glycolysis, can have many of the materials in the cycle serve a second function as triggers for cascades that signal to the nucleus and regulate genes. In dendritic cells, for example, when TLR receptors are triggered, they radically alter glycolysis pathways to produce much more energy and breakdown of materials. These changes help dendritic cells and other immune cells.
A previous post showed how these metabolic signals are a critical part of the way T cells can alter their functions so dramatically. In this case, succinate stimulates inflammation, triggering IL-1β. This alters cell compartments by providing different lipids in the membranes and structures. Similarly, other factors regulate increased and decreased inflammation, like lipoproteins LDL and CD36 modulating the inflammasome structure (the inflammasome is a large complex multi protein structure that is machinery to maintain inflammation). Omega-3 fatty acids inhibit the inflammasome and NF-κB and increase programmed cell death (autophagy). Prostoglandin E2 (well known to be involved in pain and inflammation) is involved in response to virus infections.
There are many other examples of metabolic cascades in the immune process providing more complex feedback loops. Ketone bodies (acetone, aceto-acetic acid and beta-hydroxybutyric acid) come from fatty acids and provide energy during starvation, lack of carbohydrates, extreme exercise and diet. The stimulate cytokines IL-1b and IL-18, which work against inflammation. (This may be why less calories lowers inflammation).
Inhibitors of Receptors

Special factors take off the phosphate and ubiquitin tags or stop signaling in other ways. These are enzymes involved in other processes that are stimulated specially for this task to stop inflammation that can be damaging. These enzymes, such as ubiquitin ligase and neuroregulin degradation protein (NRDP1) stop infections aimed at viruses, but at the same time stop many other cytokines that can be harmful. There are many different types that regulate the TLR receptors and maintain the general tissues from harm. There are other factors triggered by the pattern receptors that specifically stop cytokines such as IFNb
Amplifiers of Receptor Effects
Along with the many negative feed back loops and competing processes, there are specific mechanisms that increase the signal from the pattern receptors. One of these is a phosphatase enzyme.
Several pathways both strengthen and decrease the signals for cytokines in multiple ways. Some can increase the fight against viruses while limiting the over use of inflammation in the tissues. A large number of ubiquitin ligases (TRIM) have various ways that they increase the strength and length of the cytokine response.
Another mechanism involves LPS using MHC class II molecules (see post on immune and nervous system). These increase the signals in other complex pathways. There are transcription factors that also perform this function.
Many Different Signals for Innate Immunity
 There are a very large number of different dangerous particles that are picked up by pattern recognition receptors, and an even larger number of possible reactions. With all of these overlapping cascades, regulation is extremely important for the organism. In fact, these have to work together.
There are a very large number of different dangerous particles that are picked up by pattern recognition receptors, and an even larger number of possible reactions. With all of these overlapping cascades, regulation is extremely important for the organism. In fact, these have to work together.
Cooperation: There are many examples where pathways work together to increase the response. One way this occurs is by building bundles of different proteins that have similar effects but can be modified for particular situations. Some combinations work with particular bacteria others with fungus. This can work both through altering the receptors effects as well as altering the cascades that are triggered before they stimulate the cytokines.

Augmentation: These different signals can work together and greatly increase the signal. When it is determined that an even greater response is necessary these multiple pathways increase the force of the inflammation. This, most often, happens through altering specific parts of the cascade that is triggered by the receptors.
The inflammasome structure is influenced in various ways from the receptors. An example is when NF-κB is stimulated it increases the gene products of IL1B, which increases pro-IL-1β. At the same time another process alters pro-IL-1β to IL-1β. These same pathways can produce many other results. Some create a pathway where an inflammasome is established outside of the cell. These may, on their own, continue to stimulate inflammation. Communication between various inflammasomes is an important way that the signals stay enhanced.
Inhibition: The various types of receptors have ways of influencing each other in different ways. Communication between TLR and NLRs, for example, can suppress each other’s signals by complex feedback loops. Each can, also, produce states where the immune cells allow inflammation to continue or to become more careful of reactions against tissue that can be too strong. LPS is vital in these regulatory cascades that affect many different cytokines in diverse mechanisms. Most commonly, the NLR signal inhibits the TLR signal, but not always. Colitis is the result of faulty mechanisms of this type involving NF-κB cytokine.
 Another example is when flu virus increases bacterial infections through complex interactions. The response to the virus with interferon suppresses the NF-κB cytokine through a complex pathway. Also, other mechanisms contribute to this by inhibiting the ability of the tissue to fight off damage.
Another example is when flu virus increases bacterial infections through complex interactions. The response to the virus with interferon suppresses the NF-κB cytokine through a complex pathway. Also, other mechanisms contribute to this by inhibiting the ability of the tissue to fight off damage.
Positive Feedback with Complement: The complement system is a complex cascade that independently activates responses to invasion of microbes for innate immunity. The pattern receptor pathways work by themselves much of the time, but, also have interactions with complement usually with positive feedback to increase the responses. TLR can stimulate complement and complement can increase TLR responses. Some have considered that they form a complex together, but in fact the interactions are much more complex and variable including many factors that mediate both.
In one example, LPS molecules that trigger TLRs, also, stimulate complement, especially at 5a (one of the many steps of the complement cascade). The 5a and LPS work together increase many cytokines together such as TNF, IL-1β and IL-6 and NF-κB.
 Negative Feedback: In different mechanisms, NLR provide negative feedback to inhibit TLR responses. These mechanisms involve elaborate cascades using ubiquitin tags and enzymes. These can work through influencing the inflammasomes that are built to promote inflammation. One of these mechanisms is critical in the creation of rheumatoid arthritis. They involve two complex processes called pyroptosis (a special form of programmed cell death with caspace enzymes that, also, increases inflammation cytokines) and necroptosis (another type of cell death that doesn’t use caspace that causes more cytokines.)
Negative Feedback: In different mechanisms, NLR provide negative feedback to inhibit TLR responses. These mechanisms involve elaborate cascades using ubiquitin tags and enzymes. These can work through influencing the inflammasomes that are built to promote inflammation. One of these mechanisms is critical in the creation of rheumatoid arthritis. They involve two complex processes called pyroptosis (a special form of programmed cell death with caspace enzymes that, also, increases inflammation cytokines) and necroptosis (another type of cell death that doesn’t use caspace that causes more cytokines.)
Very Complex Regulation of Pattern Receptors
 Regulation involves a very large number of factors and processes. These include genetic stimulation and inhibition, epigenetic tags, alteration of proteins, control of metabolism, building of nano machines and responding to the environment. There are many factors that increase and many that inhibit processes. The risks in either direction is great—super-infection or chronic autoimmune diseases.
Regulation involves a very large number of factors and processes. These include genetic stimulation and inhibition, epigenetic tags, alteration of proteins, control of metabolism, building of nano machines and responding to the environment. There are many factors that increase and many that inhibit processes. The risks in either direction is great—super-infection or chronic autoimmune diseases.
Many of these processes converge on triggering genes of specific cytokines such as interferons and nuclear factor-κB (NF-κB). There are special regulatory factors that create many different effects at the same genes. Also, the regulation occurs differently in each different tissue of the body, and with the various kinds of immune cells involved with particular unique microbes.

Somehow, the receptors alter pathways and cascades in many different cells. These altered pathways create signals such as specific cytokines that communicate between cells and alter the processes in the other cells. These factors can be separated in the different organelles, so that these organelles are also important in the regulation. Metabolic cycles are altered that influence the rapid increase of certain types of immune cells for the job at hand.
As well as affecting genes, epigenetic tags are, also critical in these processes, making it much more complex. How do these receptors trigger these epigenetic behaviors? When specific factors alter genes, they also trigger combined use of very particular enzymes through other processes. Unique types of programmed cell death are part of these methods.
Diseases Related to Pattern Receptors
Increasingly, the processes mentioned here are found to be extremely relevant in important diseases. A short list includes diseases of the gut (inflammatory bowel disease, food allergies and damage to the gut), liver disease (viral hepatitis, metabolic cirrhosis, fibrosis, and alcoholic cirrhosis), heart disease (atherosclerosis, carditis), metabolic (diabetes, obesity) and brain (neuro inflammation, stroke, Alzheimer’s, lupus, MS, chronic pain).
Vast Complexity of Immune Pattern Recognition Receptors
 For many years, the vast array of immune responses seemed unfathomable. Discovery of complex effects of pattern receptors has greatly advanced understanding of the extremely varied responses to microbes with different kinds of inflammation. Regulation of these many different responses is just being discovered. It involves a large number of different receptors, factors and cells, including metabolic cycles.
For many years, the vast array of immune responses seemed unfathomable. Discovery of complex effects of pattern receptors has greatly advanced understanding of the extremely varied responses to microbes with different kinds of inflammation. Regulation of these many different responses is just being discovered. It involves a large number of different receptors, factors and cells, including metabolic cycles.
Where is the regulation for all of this? How can the wireless brain of the immune system coordinate such an immense regulatory network in many different cells at once and on many different orders of magnitude? Is this not an example of extraordinary cellular intelligence and inter cellular intelligence? Where does this intelligence come from?