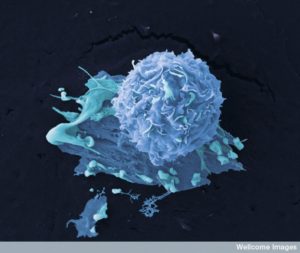
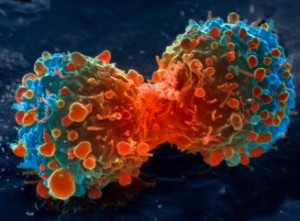
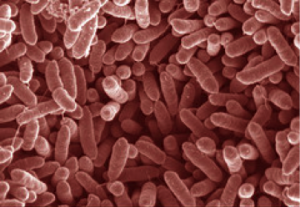
 Cancers are a community of cells that engage in continual conversations to help their cells thrive, to expand to new locations, and to fight off attacks from immune cells, microbes, and other cells. Bacteria are another community of cells that constantly talk among themselves for group activity such as finding food, defending themselves, and either helping or attacking other cells. What is very surprising is that both can converse with each other by using the same language. Using signals, they can both cooperate with each other or they can fight. It is through complex interactions and signals that cancers recruit other cells to help them such as local tissue cells, immune cells, organelles such as mitochondria (that were once microbes), and microbes. This post discusses the conversations that allow bacteria to help cancers.
Cancers are a community of cells that engage in continual conversations to help their cells thrive, to expand to new locations, and to fight off attacks from immune cells, microbes, and other cells. Bacteria are another community of cells that constantly talk among themselves for group activity such as finding food, defending themselves, and either helping or attacking other cells. What is very surprising is that both can converse with each other by using the same language. Using signals, they can both cooperate with each other or they can fight. It is through complex interactions and signals that cancers recruit other cells to help them such as local tissue cells, immune cells, organelles such as mitochondria (that were once microbes), and microbes. This post discusses the conversations that allow bacteria to help cancers.
Bacteria and Human Cancers
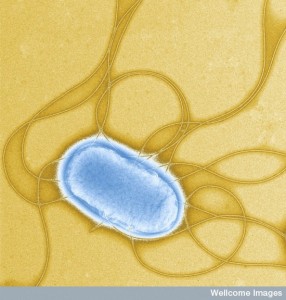
 Twenty percent of all growths in humans are aided by infections. Several viruses have been demonstrated to help change cells into cancer. In recent years, several bacteria were also found to increase cancers, but the mechanisms were not clear—H. pylori, S. enterica, and E. S. Typhi. Several other bacteria are associated with cancer but with even less understanding—C. trachomatis, F. nucleatum, and B. Fragilis.
Twenty percent of all growths in humans are aided by infections. Several viruses have been demonstrated to help change cells into cancer. In recent years, several bacteria were also found to increase cancers, but the mechanisms were not clear—H. pylori, S. enterica, and E. S. Typhi. Several other bacteria are associated with cancer but with even less understanding—C. trachomatis, F. nucleatum, and B. Fragilis.
Recently, mechanisms have been found whereby microbes via signals alter significant pathways in human cell. Some pathways in cells that have been found to be altered in this way include CagA (cytotoxin-associated gene A) in several different ways. They can alter the vital WNT and ATM (ataxia-telangiectasia mutated) pathways. They can also cause general inflammation with destruction that helps the cancers.
Many Associations of Bacteria and Cancer
 It is surprising that only 10% of tumors are caused by inherited genetic structures. The rest are caused by mutations from two sources. Some sources are signals from the environment (carcinogens), and other are errors in the mechanism that repairs DNA or that produces new cells.
It is surprising that only 10% of tumors are caused by inherited genetic structures. The rest are caused by mutations from two sources. Some sources are signals from the environment (carcinogens), and other are errors in the mechanism that repairs DNA or that produces new cells.
Millions of cancers are known to be caused by infections but the exact mechanisms are not known in many cases. Currently, only several viruses (HPV, HepB, and HepC) and one bacteria (Helicobacter pyori) are listed by the World Health Organization as definite carcinogens. But, in general, research shows infections are helping many cancers. Chlamydia infections in the lungs help lead to lung cancers and gonorrhoeae to cancers in the genital urinary system. Several others appear to cause lymphoma and are even treated by antibiotics (H. pylori, C. Jejuni, and C. psittaci). E. Coli and others appear to be related to colon and rectal cancer and a Salmonella causes a variety of gall bladder cancers.
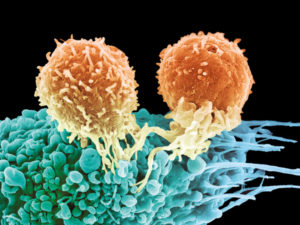
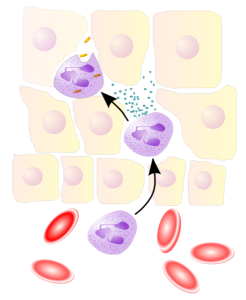
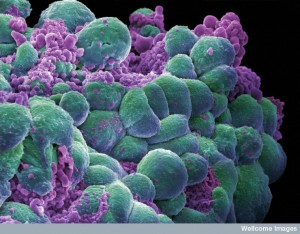 It takes years and many steps to start a cancer, so it is not obvious how this happens. There are many different factors that move this process along. One is for the cell to find a way to avoid signals that would normally kill an abnormal cell (programmed cell death or apoptosis). Another is to avoid factors that all cells have to stop cancers (growth suppressors). Another important aspect it to signal for an increase in growth and production, much as the T cell (This process has been described in posts on cancer and T cells where the metabolism of the cell is used as signals to genetic networks to alter cellular shape and activity.) Finally, they must stop normal cell aging through alteration of the chromosomes and develop the ability to eternally divide.
It takes years and many steps to start a cancer, so it is not obvious how this happens. There are many different factors that move this process along. One is for the cell to find a way to avoid signals that would normally kill an abnormal cell (programmed cell death or apoptosis). Another is to avoid factors that all cells have to stop cancers (growth suppressors). Another important aspect it to signal for an increase in growth and production, much as the T cell (This process has been described in posts on cancer and T cells where the metabolism of the cell is used as signals to genetic networks to alter cellular shape and activity.) Finally, they must stop normal cell aging through alteration of the chromosomes and develop the ability to eternally divide.
Changes that Lead to Cancer
 As these changes occur, cells alter vital pathways for normal cell function. These important branch points have been given the name of “checkpoints”. An important checkpoint controls repair of damaged DNA. Cancer wants chaos and instability in the genes so that more mutations can develop, some of which will help the cancer. The cancer cells are awaiting vital changes to help them. Changes:
As these changes occur, cells alter vital pathways for normal cell function. These important branch points have been given the name of “checkpoints”. An important checkpoint controls repair of damaged DNA. Cancer wants chaos and instability in the genes so that more mutations can develop, some of which will help the cancer. The cancer cells are awaiting vital changes to help them. Changes:
- that affect signaling of damage (the DNA damage response or DDR),
- the extremely important WNT pathway that controls aspects of making RNA from DNA and especially proteins for apoptosis versus cell division. (The name WNT comes from pathways wingless in flies and int in mice)
- enzymes called kinases that are part of vital pathways similar to WNT (MAPK, AKT),
- the cytokine interferon that signals to the nucleus regulating and responding to making blood vessels, cell movement, defense against invasion, and cell death, and
- inflammation cytokines that stop apoptosis (nuclear factor-κB (NF-κB),
Stopping normal immune responses allows the cancer to grow out of control. Bacteria cause cancers in many ways, it turns out. They can directly alter these important signals with their own communication or damage DNA directly. They can have other local and blood effects. Research is showing altering cell lines in the lab dishes by signaling from bacteria. They can use manipulation of the DNA damage response (DDR) pathway and those pathways that increase growth. Indirect pathways are producing stress with oxidation metabolites, microbe signaling in the gut, altering immune responses, and the many different effects of inflammation
Bacterial Toxins that Damage DNA
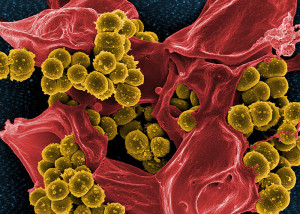
 When DNA is disrupted, the many checks and balances against abnormal activity are affected. Unstable genetic activity leads to alterations or absent DNA code letters that can alter and stop the powerful tumor suppressors. The opposite can happen where special genes are triggered that enhance cancers, called oncogenes. There are so many different kinds of bacteria in the gut (more than the number of human cells) and they produce products from 300 times the amount of DNA in human cells that some secret toxins that affect DNA damage.
When DNA is disrupted, the many checks and balances against abnormal activity are affected. Unstable genetic activity leads to alterations or absent DNA code letters that can alter and stop the powerful tumor suppressors. The opposite can happen where special genes are triggered that enhance cancers, called oncogenes. There are so many different kinds of bacteria in the gut (more than the number of human cells) and they produce products from 300 times the amount of DNA in human cells that some secret toxins that affect DNA damage.
Four products that help produce cancers in particular are well documented: colibactin from E. Coli; cytolethal distending toxin or CDT from gram negative bacteria; Shiga toxin from Shigella dysenteriae; and endonucleases from N. gonorrhoeae.
1. Colibactin toxin is the most studied. It is produced by a particular genetic network called a genomic island (pks), which is also in other related species. Genomic islands are passed through horizontal gene transfer. This region of genes produces several different kinds of enzymes (polyketide synthases and an unusual enzyme not produced by ribosomes, that along with eight other proteins produce this complex toxin. E. coli can live for a long time in the colon and can eventually produce colon and rectal cancers. These toxins break both strands of DNA (double stranded breaks or DSBs). These produce a cascade of very complex events involving histones, and several additions of phosphorus (by kinase enzymes).
 The reproduction cycle is interfered with–at first stopped, then partially repaired in a way that allows mutations and cancer development. The genes remain unstable and enter into a special aging pathway (senescence-associated secretory phenotype or SASP – see post of how cells stop their own aging when part of infection.)
The reproduction cycle is interfered with–at first stopped, then partially repaired in a way that allows mutations and cancer development. The genes remain unstable and enter into a special aging pathway (senescence-associated secretory phenotype or SASP – see post of how cells stop their own aging when part of infection.)
Most people are unaware that cells can affect their own aging. (see previous post). In one mechanism they are deliberately rapid agers so that scars won’t form after healing of inflammation. But, in this case, signals go out to increase inflammation and tell other cells to rapidly reproduce. These factors are signals that help the tumor get larger by affecting all of the cells in the neighborhood. A previous post on cancer showed how cancers get all of the local tissue cells involved to help and this is one mechanism.
These also affect the very important pathway for protective cell death regulated by the vital proteins p53 and p21. This process affects two vital checkpoints (T1-S to avoid copies of damaged DNA and G1-M to avoid abnormal cell division).
 2. CDT (cytolethal distending toxin) attacks the DNA as well. This toxin has three parts (A, B, and C) that are manufactured together. B has the active sequence and uses A and C to get into the human cell. Cells pick it up in vesicles and transport it backwards to the cell’s endoplasmic reticulum (the ER is the organelle that makes proteins from ribosomes and folds and activates them).
2. CDT (cytolethal distending toxin) attacks the DNA as well. This toxin has three parts (A, B, and C) that are manufactured together. B has the active sequence and uses A and C to get into the human cell. Cells pick it up in vesicles and transport it backwards to the cell’s endoplasmic reticulum (the ER is the organelle that makes proteins from ribosomes and folds and activates them).
Like a viral manipulation, the ER breaks it down and sends it into the nucleus. There it causes double DNA breaks and affects both check points mentioned above that would normally avoid copies of abnormal DNA and avoid abnormal cell division. It does this in many kinds of cells—fibroblasts and immune cells. But, in lining cells (endothelial) it tricks the check points and only temporarily stops their activity. Therefore, abnormal DNA is copied and abnormal cells are dividing.
Both Colibactin and CDT also stimulate more inflammation and many cytokines that help increase inflammation and therefore the cancer (interleukin IL-6, IL-8, TNF, interferon, and NF-κB and many others). After a while there is greater and greater chance of cancer developing in this complex situation. Also, vital proteins that stop programmed cell death are produced including BCL-2 and others. All these factors increase cell growth.
Another pathway is sometimes affected—the vital DDR (DNA damage response) through the very complex cascades of the vital ATM and MAPK pathways. This helps to move cells into new places as they cancer grows.
CDT uses all these means to cause DNA havoc and produces abnormal cells that are reproducing faster with abnormal mutations present. Statistically, this can lead to active cancers.
3.  Another protein factor is called uropathogenic-specific protein (Usp gene) from E. coli. Another island of genes produces Usp. It has actions in endothelial lining cells that produce cancers also. But, the mechanism isn’t worked out. It is part of many colibactin bacteria as well.
Another protein factor is called uropathogenic-specific protein (Usp gene) from E. coli. Another island of genes produces Usp. It has actions in endothelial lining cells that produce cancers also. But, the mechanism isn’t worked out. It is part of many colibactin bacteria as well.
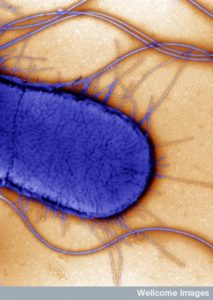
4. Exoenzyme S toxin of Pseudomonas aeruginosa, a gram negative bacteria that is often in people with cystic fibrosis. This bacterium uses the complex syringe like type III secretion system to inject the toxin into human cells. (Please see the post on these incredibly complex machines built by bacteria.) In lung cells and macrophages it affects the p53 programmed death pathway, and also causes breaks in double stranded DNA.
All of these toxins kill off immune cells that are rapidly reproducing like killer T cells. And support
Bacteria Manipulating DNA Damage Responses
 Bacteria both increase DNA breaks, but also disrupt the damage response. They can manipulate vital proteins that repair DNA damage and the vital p53 pathway. These inhibit the checkpoints and the repair process causing gene disruption that is then copied into other new cells.
Bacteria both increase DNA breaks, but also disrupt the damage response. They can manipulate vital proteins that repair DNA damage and the vital p53 pathway. These inhibit the checkpoints and the repair process causing gene disruption that is then copied into other new cells.
P53 is the most well-known and perhaps the most important molecule that suppresses and stops cancers from developing. It is produced from the gene TP53 and is normally metabolized by an enzyme (MDM2 E3 ubiquitin ligase). When the cell has stress, p53 is maintained longer and triggers genetic networks making proteins that stop the reproduction cycle, triggers programmed cell death, and stops some metabolic pathways (pentose phosphate pathway). Half of cancers have a mutation in the gene that produces p53 stopping its work and helping cancers. Many viruses that cause cancers alter p53 (HPV, HepB, HepC, and EBV.)
Chlamydia trachomatis is transmitted with sex and infects 100 million new people a year. It lingers without symptoms and damages DNA through epigenetic mechanisms caused by reactive oxygen species (ROS) metabolic products. A pathway is stimulated by ROS which increases cell growth and helps more bacteria to enter cells. By another pathway it damages p53 as well. By altering p53 certain metabolites are produced that help the bacteria. This alteration of metabolism allows cancer cells to grow when there is little oxygen (Warburg effect). This is similar to the metabolic state of the activated T cell when it has to travel widely without oxygen.
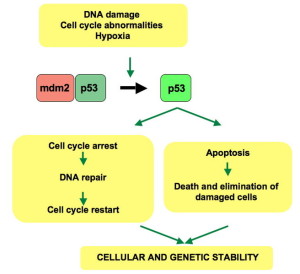 Shigella in the gut also increases the metabolism of p53 by several different mechanisms. These infected cells can repair DNA damage somewhat but the DDR process actually increases mutations that are carried on. H. pylori infects a large number of people and only stimulates stomach cancer in some people.
Shigella in the gut also increases the metabolism of p53 by several different mechanisms. These infected cells can repair DNA damage somewhat but the DDR process actually increases mutations that are carried on. H. pylori infects a large number of people and only stimulates stomach cancer in some people.
It appears that there are many interacting factors including food, immune, and lining cells that determine whether cancer develops. A genetic island (cag pathogenicity island or cag-PAI) makes a protein and a type IV secretion system to inject the protein. This protein and secretion connections with a human protein (integrin-b1) and then interacts with the cytokine NF-κB. All these together stimulate the DDR and at the same time there are three very complex ways H. pylori targets p53 and degrades it.
Neisseria gonorrhoeae has enzymes that cause DNA breaks. It affects another pathways p21 and p27 and inhibits the checkpoint. It evades the checkpoints and causes double DNA breaks.
Direct Action on the DDR.
Multiple mechanisms attack the cellular responses to fix damaged DNA.
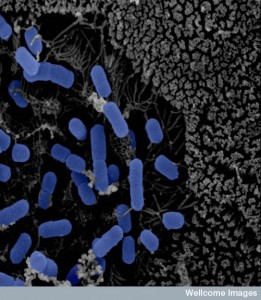
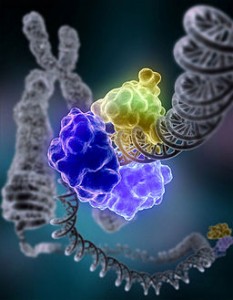 A very complex multi protein machine is used by human cells to notice DNA breaks and mobilize the DNA repair mechanisms (DDR). Listeria comes from food and causes double DNA breaks. By totally different mechanisms than the DNA breaks, it damages the complex and increases mutations.
A very complex multi protein machine is used by human cells to notice DNA breaks and mobilize the DNA repair mechanisms (DDR). Listeria comes from food and causes double DNA breaks. By totally different mechanisms than the DNA breaks, it damages the complex and increases mutations.
Another mechanism repairs DNA that is altered by accident during copying of DNA when cells reproduce (DNA mismatch repair or MMR). Many colon cancers have this type of problem. E. coli produces proteins injected into cells that alters this repair process. This injected bacterial protein alters the ability of immune cells to eat microbes (phagocytosis), damages mitochondria, and the ability of lining cells to stay tight in junctions. It alters MMR by damaging several of its proteins and increases mutations, as in colon cancer. (See previous post on Cellular Self Editing of DNA).
Bacteria Attack and Alter Cellular Signals
 Certain vital pathways are targeted by bacteria to disrupt the cell—AKT, MAPK and WNT.
Certain vital pathways are targeted by bacteria to disrupt the cell—AKT, MAPK and WNT.
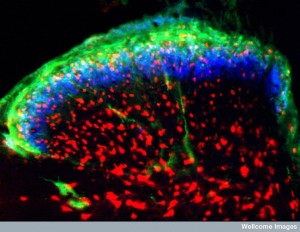
The WNT-b-catenin pathway regulates stem cell functions and decisions these cells make about what cell is produced. The pathway is abnormal in stomach and colon cancers. H. pylori has a group of genes that make variations in regions of the toxins produced. Very complex pathways effect the ability of gut cells to maintain the barrier region. This produces changes in the epithelial cells that eventually become cancerous.
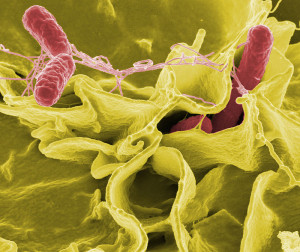
Salmonella makes a toxin that is injected by III secretion system and targets this same pathway in different ways. It stimulates particular oncogenes MYC. They cause lining cells to multiply in abnormal ways. Fusobacterium in the mouth is related to periodontal disease and problems in childbirth including stillbirth. It can also be in the gut and with infections, it is involved in colon cancer. Its toxin targets a receptor on the membrane that triggers WNT in abnormal ways. Bacteroides fragilis in the gut is part of inflammation of the colon (colitis). Its toxin can interact with WNT as well.
 MAPK and AKT also vital pathways that are often triggered with infection of H. pylori and Typhi and affect growth, programmed cell death, rapid reproduction, and cellular travel. H. pylori influences these pathways in multiple different complex ways with different poteins. One signal limits T helper 17 responses. The infection stimulates gut cells to make the signal IL-17, which triggers pathways then IL-8, which triggers more inflammation.
MAPK and AKT also vital pathways that are often triggered with infection of H. pylori and Typhi and affect growth, programmed cell death, rapid reproduction, and cellular travel. H. pylori influences these pathways in multiple different complex ways with different poteins. One signal limits T helper 17 responses. The infection stimulates gut cells to make the signal IL-17, which triggers pathways then IL-8, which triggers more inflammation.
A molecule on the H. pylori membrane triggers other cytokines and pathways that also stimulate more IL-8 and more inflammation. A very complex cascade produces a protein which stops apoptosis or programmed cell death, causing more abnormal cells to multiply. Yet another mechanism at the same time inhibits other tumor suppressors. Another pathway produces prostaglandin E2 (PGE2), which is sent outside the cell where it triggers receptors on the surface of the cell causing cytokines that make more blood vessels for the cancer.
These extremely complex mechanisms create signals that increase the entry of more bacteria, decrease of immune cells, cause more inflammation and the production of abnormal cells, and stop tumor suppression—all helping cancer development.
 Salmonella Typhi lives in the gall bladder and liver and helps produce gall bladder cancer. This occurs mostly in India and Pakistan. The same pathways for H. pylori increases the uptake of more bacteria. They stimulate genes that make cancer and inhibit p53.
Salmonella Typhi lives in the gall bladder and liver and helps produce gall bladder cancer. This occurs mostly in India and Pakistan. The same pathways for H. pylori increases the uptake of more bacteria. They stimulate genes that make cancer and inhibit p53.
Bacteroides produces toxins that stimulate inflammation of the colon and tumors. It also stimulates IL-8 and stops programmed cell death allowing cells to mutate and reproduce with these abnormalities.
All of these bacteria alter the conversations in human cells so that more bacteria are invited into the cell. They then alter major pathways that allow DNA damage and abnormal cells to multiply. Only a small percentage of cells actually transform into cancers.
Indirectly Causing Cancers
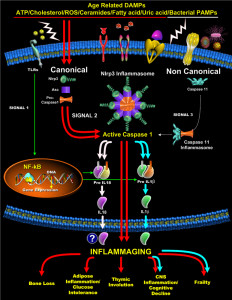
 Bacteria cause cancer in another way. They can cause a long standing inflammation that allows altered DNA to accumulate. It can also stress the cell so the reactive oxygen accumulates altering the cell (ROS). ROS increases DNA breaks and mutations. Other causes of ROS are radiation, ultraviolet light, and inflammation all of which cause DNA mutations, sometimes leading to cancers.
Bacteria cause cancer in another way. They can cause a long standing inflammation that allows altered DNA to accumulate. It can also stress the cell so the reactive oxygen accumulates altering the cell (ROS). ROS increases DNA breaks and mutations. Other causes of ROS are radiation, ultraviolet light, and inflammation all of which cause DNA mutations, sometimes leading to cancers.
Chlamydia trachomatis increases ROS by producing a protein that alters mitochondria. By changing mitochondria metabolism there is more ROS. Another species produces hydrogen peroxide from metabolism of polyamines. These cause DNA damage and more tumors. In fact, hydrogen peroxide can seep into cells and cause DNA damage, while programmed cell death is inhibited creating abnormal cells that multiply.
Another source of cancer transformations comes from the gut where metabolites of food alter immune pathways (see post). These microbe products come from metabolism of fiber in food, proteins, and bile acids. These alter immune response, programmed cell death, and cell multiplication. One of these (DCA or deoxycholic acid) affects liver cells to produce cytokines and factors that increase liver cancers.
Chronic infection increases the chances of cancers even in regions not near the inflammation. Examples are signals from the gut that alter liver cells. Cytokines that increase inflammation aid this process with ROS production and other factors that help cells grow, even abnormally (WNT as above). This can also stimulate the process in the prostate. Gut microbes help liver cancer in three distinct ways—cytokines causing inflammation, factors from microbes that affect the cell’s membrane, and altering bile acid metabolism.
When the immune system is less responsive, the checkpoints are more affected and the immune responses are bypassed. Cancer treatments that inhibit immune checkpoints use this for treatment of melanoma. Bacteria decrease immune responses for their own advantage. This decreases control of cancer cells that evade the immune system.
How Do Bacteria Help Cancers
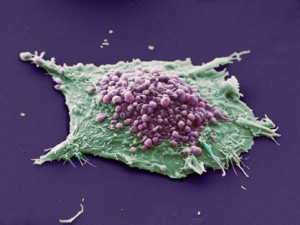 New advanced cancer treatments have to alter the conversations of bacteria and human cells. Bacteria produce one or more of the steps necessary to produce cancer, which is why most infected people don’t develop cancers. Those who have long standing infections, such as tuberculosis, become more likely to produce cancers.
New advanced cancer treatments have to alter the conversations of bacteria and human cells. Bacteria produce one or more of the steps necessary to produce cancer, which is why most infected people don’t develop cancers. Those who have long standing infections, such as tuberculosis, become more likely to produce cancers.
Bacteria produce more DNA damage, alter signals of human cells, avoid immune responses while triggering inflammation, and producing products (carcinogens) from foods or digestion that help cancer development. The effects of all of these complex pathways increases cell survival, alters neighboring cells to help, alters and suppresses the immune system, and increases genetic instability and mutations.
Studying bacterial effects on cancer are very complex, because there is no one clear mechanism. But, rather many different circumstances makes it impossible at this time to determine exactly which microbes are carcinogenic and which aren’t. All of these interactions are based on the natural communications between bacteria and human cells.