 The short answer is by very complex intelligent communication with a vast array of signals from a single layer of cells. This single intestinal epithelial cell layer makes elaborate decisions about digestion, types of diet, analysis of the effects of trillions of microbes and the types of immune cells and specialized lymph nodes. What are the mechanisms that allow one cell to understand all of the factors involved?
The short answer is by very complex intelligent communication with a vast array of signals from a single layer of cells. This single intestinal epithelial cell layer makes elaborate decisions about digestion, types of diet, analysis of the effects of trillions of microbes and the types of immune cells and specialized lymph nodes. What are the mechanisms that allow one cell to understand all of the factors involved?
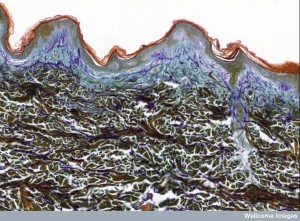
The barrier cells in the skin, gut and blood-brain do much more than block microbes and toxins from entering the body. These intelligent epithelial cells engage in elaborate back and forth communication with the trillions of microbes on the outside as well as many different kinds of immune cells on the inside. The communication determines which microbes are considered friendly, which are drawn nearby for protection, which are allowed to make vitamins and other factors and which are enemies that need particular immune responses.
 Signaling of epithelial cells with immune cells determines which types are needed and how the immune centers and factories in lymph nodes and specialized tissues are formed. See the posts on the intelligent skin cell and the intelligent intestinal epithelial cells for more information than is in this post. Perhaps, the most intelligent of all of these epithelial cells is the choroid cells that allow only very small molecules (one eighth the size of the intestinal cell) and very particular microbes and cells to enter the brain. Choroid cells determine the constitution of the cerebral spinal fluid, including responding to signals from every part of the brain and sending exact messages to attract the type of immune cell needed for any current brain region problem. (See post on intelligent choroid cell).
Signaling of epithelial cells with immune cells determines which types are needed and how the immune centers and factories in lymph nodes and specialized tissues are formed. See the posts on the intelligent skin cell and the intelligent intestinal epithelial cells for more information than is in this post. Perhaps, the most intelligent of all of these epithelial cells is the choroid cells that allow only very small molecules (one eighth the size of the intestinal cell) and very particular microbes and cells to enter the brain. Choroid cells determine the constitution of the cerebral spinal fluid, including responding to signals from every part of the brain and sending exact messages to attract the type of immune cell needed for any current brain region problem. (See post on intelligent choroid cell).
Recent research shows that many different micronutrients from the diet are critical parts in this decision making process. This type of signaling between epithelial and immune cells is necessary to develop immunity for babies that determine life long immunity. Micronutrients and the epithelial signaling are, also, vital in a day-to-day basis to maintain the various immune cells needed for each circumstance throughout life. Vitamins A and D have been known to be extremely important for immunity, but the mechanisms have not been clear. Recent research has discovered special receptors and cascades into the nucleus that are used by these vitamins and are needed for immunity. Along with these two vitamins, many other molecules from food trigger these vital pathways and interact in the nucleus through additional special nuclear receptors. Micronutrients in fruits and vegetables are just being discovered and the mechanisms are extremely complex.
This post will describe recently discovered mechanisms of signaling in the gut epithelial cells that determine the unique lymphocytes and lymph tissues needed to fight infections throughout life. As more is learned, this line of research will map the extremely complex relationship of diet and life long immunity, which is completely dependent on intelligent communications between these cells.
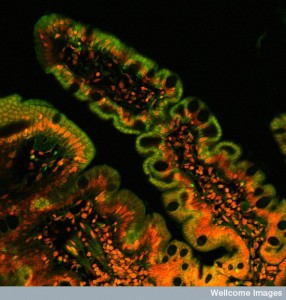
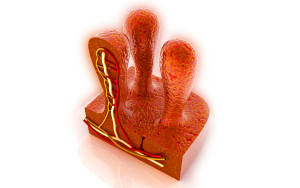
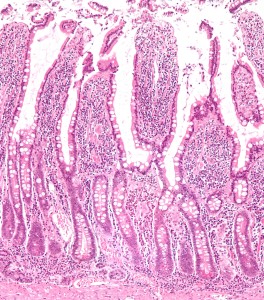
Intestinal Epithelial Cell
 The very intelligent intestinal epithelial cell was discussed in a previous post. This section is a brief summary of material in that post. The gut has been considered a second brain with the largest semi autonomous nervous system outside of the brain. Much of this activity is coordinated in this one layer of epithelial cells.
The very intelligent intestinal epithelial cell was discussed in a previous post. This section is a brief summary of material in that post. The gut has been considered a second brain with the largest semi autonomous nervous system outside of the brain. Much of this activity is coordinated in this one layer of epithelial cells.
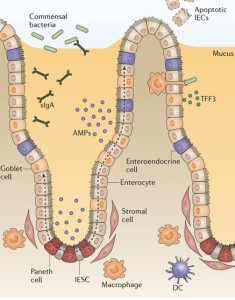
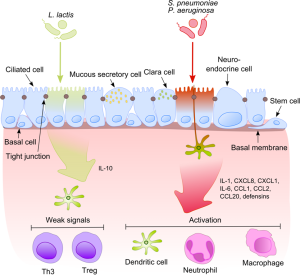
In most areas, microbes trigger vigorous immune responses. In the intestine, epithelial cells play a critical role in deciding whether a modified response or no response should occur, instead. Cascades of molecules that trigger genetic networks are involved in making the decision to produce graded immune responses. Friendly microbes signal for protection from infection and tissue damage, but this friendly signaling can increase cancer creation. The epithelial cell must balance digestion, protection against dangerous microbes, support of friendly microbes, modulation of inflammation and avoiding cancer. Different responses occur in different parts of the bipolar shaped cell.
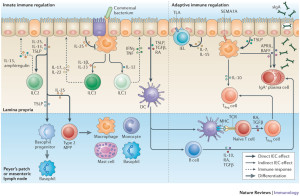
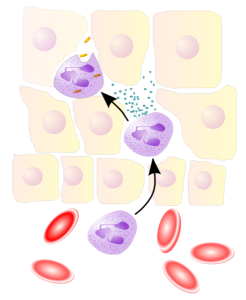
Epithelial cells are in constant communication with immune cells, such as phagocytes that present antigens to T cells. These signals either increase or decrease the amount of dendritic cells and macrophages that will tolerate friendly bacteria. In fact, there are a wide variety of different kinds of phagocytes that travel to the various lymph nodes with microbe antigens–both live bacteria and pieces of microbes. Because they hang out at the barrier lamina, some of these macrophages already understand tolerance to some microbes.
 Messages from the barrier epithelial cells instruct traveling T cells to be tolerant or not. The macrophage can signal with cytokines that loosen the tight junctions and allow them to stick their long arms through to the lumen to grab particular antigens to be analyzed, defeated or helped. In fact, the epithelial cell initiates the signals to the tight junction. Other functions are:
Messages from the barrier epithelial cells instruct traveling T cells to be tolerant or not. The macrophage can signal with cytokines that loosen the tight junctions and allow them to stick their long arms through to the lumen to grab particular antigens to be analyzed, defeated or helped. In fact, the epithelial cell initiates the signals to the tight junction. Other functions are:
- Interacting positively and negatively with trillions of microbes using thousands of cytokine signals
- Modulating the immune system to accommodate thousands of different microbe communities
- Determining multiple attributes of digestion of food and production of vitamin
- Influencing the human immune system development and normal function through thousands of cytokines
- Signaling in complex ways to many types of cells with thousands of cytokines
- Maintaining order by building and supporting the barrier that separates the microbes from the body
- Producing enzymes to help or hurt microbes
- Producing mucous that creates a barrier region for friendly microbes
Exposure to the Environment
 Exposure to the environment is a double-edged sword for organisms. They need the nourishment and must avoid toxins, dangerous microbes and assault. The immune system is the first responder for invasion by microbes and toxins and the response to injury. The immune system consists of a very large number of different types of cells that are called upon for a vast amount of different tasks (including the vast number of different bacteria and viruses). These cells are unique in particular organs. At the skin (see post), intestinal (see post) and respiratory epithelium, a conversation occurs between the outside world of trillions of microbes and inside world of necessary types of immune cells. The external influences are part of this conversation and influence how immune cells and their lymph structures develop and perform. Perhaps, the most significant influence from the environment is the food and drink that are necessarily taken in. In this way, specific nutrients, such as vitamin A, can have many varied effects in different locations. This research is the new frontier of diet influencing inflammation.
Exposure to the environment is a double-edged sword for organisms. They need the nourishment and must avoid toxins, dangerous microbes and assault. The immune system is the first responder for invasion by microbes and toxins and the response to injury. The immune system consists of a very large number of different types of cells that are called upon for a vast amount of different tasks (including the vast number of different bacteria and viruses). These cells are unique in particular organs. At the skin (see post), intestinal (see post) and respiratory epithelium, a conversation occurs between the outside world of trillions of microbes and inside world of necessary types of immune cells. The external influences are part of this conversation and influence how immune cells and their lymph structures develop and perform. Perhaps, the most significant influence from the environment is the food and drink that are necessarily taken in. In this way, specific nutrients, such as vitamin A, can have many varied effects in different locations. This research is the new frontier of diet influencing inflammation.
 Signaling at the epithelial lining is perhaps the most sophisticated of any in the body. A wide variety of signals back and forth help determine which microbes will be supported as friends and which will be fought as enemies. The signals involve both cytokines and neurotransmitters. There are a variety of microbes that are absolutely necessary for production of needed materials and vitamins. It is known that diet affects immunity and general health (research in poor countries), but only recently has the particular molecular events been understood. It affects diabetes, heart disease and cancer. Recent research shows elaborate signaling from microbes and many parts of the body.
Signaling at the epithelial lining is perhaps the most sophisticated of any in the body. A wide variety of signals back and forth help determine which microbes will be supported as friends and which will be fought as enemies. The signals involve both cytokines and neurotransmitters. There are a variety of microbes that are absolutely necessary for production of needed materials and vitamins. It is known that diet affects immunity and general health (research in poor countries), but only recently has the particular molecular events been understood. It affects diabetes, heart disease and cancer. Recent research shows elaborate signaling from microbes and many parts of the body.
Because of the constant assault by toxins, situations are closely observed by the travelling and tissue resident immune cells. Toxins and dangerous microbes are identified by receptors on T and B-lymphocytes in the lymph tissues near these gateway organs, especially the GI tract.
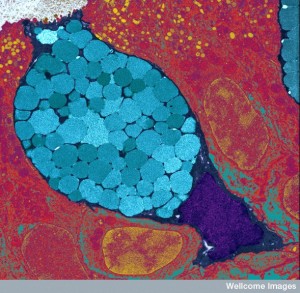
Specialized immune cells in the small intestine include two types of intraepithelial lymphocytes (IELs). They have T cell receptors (TCRs) and can rapidly respond to danger, but meanwhile, maintain the barrier and the tissue. They produce IFN-γ, which rapidly kills enemy cells, but can’t produce IL-17. They are present at birth helping to deal with the very first microbes. They can suddenly change to become memory T cells.
Further below the entrance at the epithelial cell, there are many other different types of immune cells including many distinct T helper cells, which can produce IL-17 to protect against fungus. These unique cells don’t occur in other places in the body. But, this cytokine is implicated in multiple sclerosis, rheumatoid arthritis and lupus. Sodium chloride levels can influence this cytokine. (See post on Intelligent T Cells.)
Lymph Tissue is the Home Base and School for Lymphocytes
Peyer’s patches, which are large lymph tissues exposed to the outside world, and internal lymph nodes are the places where lymphocytes identify and start reacting to specific molecules (antigens) by producing new specialized types of cells. They must identify the good bacteria and molecules from the organism (self molecules) and keep the organism tolerant, that is, avoid a destructive reaction to them. If they don’t function well, they can become a place where viruses can live chronically. Because these systems develop in the fetus, factors from the environment can begin their influence before birth, by producing particular kinds of lymph structures.
After birth, a unique type of small lymph structure (cryptopatche) appears in the intestine just under the crypts of Lieberkun, where villi are formed. When they are exposed to microbes, they become adult isolated lymphoid follicles (ILFs) that produce lymphoid tissue initiator cells (LTin cells) and lymphoid tissue inducer cells (LTi cells). As these cells respond to more and more microbes and other materials, the cryptopatches mature.
Early Diet is Very Important
 Studies of poor countries have found that nutrition is critical for the proper response to vaccinations. Studies now show that response to micronutrients includes both the central thymus organ and other lymph nodes. Specific nutrients are necessary for the fetus to develop good immune structures and cells. Also, specific diet is necessary after birth for the cryptopatches to develop normally. In particular, vitamin A influences the size of fetus lymph nodes and Peyer’s patches in mice through the vitamin A receptor—retinoic acid receptor (RAR alpha). Stimulating this receptor is essential for immune function later in life, particularly against viruses. This influence appears to be from the LTi cells, not B and T-lymphocytes and cannot be reversed later in life.
Studies of poor countries have found that nutrition is critical for the proper response to vaccinations. Studies now show that response to micronutrients includes both the central thymus organ and other lymph nodes. Specific nutrients are necessary for the fetus to develop good immune structures and cells. Also, specific diet is necessary after birth for the cryptopatches to develop normally. In particular, vitamin A influences the size of fetus lymph nodes and Peyer’s patches in mice through the vitamin A receptor—retinoic acid receptor (RAR alpha). Stimulating this receptor is essential for immune function later in life, particularly against viruses. This influence appears to be from the LTi cells, not B and T-lymphocytes and cannot be reversed later in life.
There is still little information on exactly what type of nutrition is absolutely necessary at certain points in development. It comes from various foods and involves a lot more than the known vitamins. In fact, impairments that occur in the immune response to vaccines are dependent on micronutrients. These problems with the strength of vaccinations cannot be reversed later. Mothers who are undernourished have less immunoglobulin A.
In cultures where the quality of nutrition is tied to the harvest cycle, those born at the time of harvest have less mortality from infections as adults. Exposure to sunlight and vitamin D contributes to better immunity. These factors influence the number and size of lymph nodes that develop, including Peyer’s patches in the gut, just below the epithelial cell. The immune cells in the nodes benefit from some of the microbe products from the lymph and blood flow. The LTi cells start building the nodes before birth, when vitamin A is critical. The cryopatches appear at birth and grow based on signals from the epithelial cells, immune cells and microbes.
Vitamin A
 Vitamin A comes from animal and plant food and is only rare in poor countries, where children develop night blindness as an early symptom of vitamin A deficiency. Plants have an inactive molecule (beta-carotene) that is oxidized by enzymes to retinol, which is taken into cells. Enzymes in the epithelial cells then makes trans-retinoic acid and 9-cis-retinoic acid. Animals have an active form of vitamin A in fat that can be built up to toxic levels. Retinoic acid is fat-soluble and diffuses easily. Also, epithelial and intestinal immune cells, dendritic cells make retinoic acid, as well as directing lymphocytes.
Vitamin A comes from animal and plant food and is only rare in poor countries, where children develop night blindness as an early symptom of vitamin A deficiency. Plants have an inactive molecule (beta-carotene) that is oxidized by enzymes to retinol, which is taken into cells. Enzymes in the epithelial cells then makes trans-retinoic acid and 9-cis-retinoic acid. Animals have an active form of vitamin A in fat that can be built up to toxic levels. Retinoic acid is fat-soluble and diffuses easily. Also, epithelial and intestinal immune cells, dendritic cells make retinoic acid, as well as directing lymphocytes.
Children from poor countries with poor diets that have low weight have many more infections from a poorly developed immune system. It is still a big problem in Asia and Africa despite programs to increase vitamin A for pregnant women. By the time, the children are born it is too late for vitamin A to reverse the life long immune problems. Even increased amounts after birth did not help reverse the problems, even though it is absolutely necessary for survival.
 As well as helping to develop appropriate lymph tissue in the fetus, vitamin A has important effects in maintaining appropriate lymphocytes and other immune cells (TCRs) in the intestines. The size of the stem cell pool that makes the special lymphocytes sitting in the intestinal epithelium appears to be determined in the fetus and stays poor throughout life, if it is deficient at birth. It also limits the other lymph organs. It is not yet known exactly where the IELs, lymphocytes that sit in the intestinal epithelium, are made.
As well as helping to develop appropriate lymph tissue in the fetus, vitamin A has important effects in maintaining appropriate lymphocytes and other immune cells (TCRs) in the intestines. The size of the stem cell pool that makes the special lymphocytes sitting in the intestinal epithelium appears to be determined in the fetus and stays poor throughout life, if it is deficient at birth. It also limits the other lymph organs. It is not yet known exactly where the IELs, lymphocytes that sit in the intestinal epithelium, are made.
Vitamin A is also critical to T cells and their functions in general. It appears to be critical for special T regulator cells to form all through the body. Vitamin A stabilizes some T cells when they are fighting infections. It stops them from becoming the negative type of T cell. This means that Vitamin A is critical in the fetus but all through life, as well. Vitamin A is used differently when there are different sets of nutrients being ingested.
The Aryl Hydrocarbon Receptor
 There are a variety of receptors discovered for vitamin A and D as well as other micronutrients.
There are a variety of receptors discovered for vitamin A and D as well as other micronutrients.
Recently, a very important receptor family was discovered—the arylhydrocarbon receptors AhRs. These are critical in the response to the environment and respond to many different substances in different ways. One receptor picks up toxins like dioxin, which has negative effects on the immune system including the thymus. Others respond to products from apples (quercetin), resveratrol in grapes and curcumin with positive effects. This process is important for LTi cells to stimulate the proper cryopatches and mature isolated lymphoid patches ILFs. Animals, not fed these vegetables, did not have enough immune function to fight off infections. The research is not conclusive yet that these factors cannot reverse some of the immune problems later.
 AhRs are important in T regulator cells in the regions below the epithelial cells. Stimulating these AhRs from the diet factors is necessary to have the cytokine IL-22 that is critical for the epithelial cells to prosper. These AhRs are also critical for the lymphocytes that live in between the epithelial cells. In fact, without AhR stimulation there are very few of them.
AhRs are important in T regulator cells in the regions below the epithelial cells. Stimulating these AhRs from the diet factors is necessary to have the cytokine IL-22 that is critical for the epithelial cells to prosper. These AhRs are also critical for the lymphocytes that live in between the epithelial cells. In fact, without AhR stimulation there are very few of them.
AhR is a critical receptor in many different immune cells; it was first identified in several types of T cells. It is important for the stimulation of the cytokines IL-17 and IL-22 cytokines. There are many different chemicals that can stimulate these receptors in various ways. These AhR receptors have evolved over time to be able to respond to even modern totally new chemicals. Some immune cells have the inability to function without these receptors. Without these receptors there is more dangerous inflammation and less of the critical lymphocytes in the intestine.
AhR receptors also exist in the epithelial cells of the intestine where they respond to a wide range of products from microbes and appear to be one of the main ways that epithelial cells deal with microbes. In this role they increase the immune functions of cells that may not even be traditional immune cells.
 In diets fed to mice with all known micronutrients and vitamins, but no natural fruits and vegetables with their unique compounds, the number of lymphocytes in the total intestine was decreased (but not in the epithelial cells). But, if they were given a product indole I3C that exists in broccoli, Brussels sprouts, kale and cabbage they were maintained. This product doesn’t trigger AhRs itself but instead makes a variety of other active molecules that do (such as diindolylmethane or DIM).
In diets fed to mice with all known micronutrients and vitamins, but no natural fruits and vegetables with their unique compounds, the number of lymphocytes in the total intestine was decreased (but not in the epithelial cells). But, if they were given a product indole I3C that exists in broccoli, Brussels sprouts, kale and cabbage they were maintained. This product doesn’t trigger AhRs itself but instead makes a variety of other active molecules that do (such as diindolylmethane or DIM).
AhRs and Response to Inflammation

There is still little known about the human AhR receptors and what food products stimulate them, even though it is clear that green vegetables and some microbes do. Without AhRs, mice develop colitis and other infections with many inflammation related changes. These changes include increased cytokines, scarring and microbes.
Studies show that irritable bowel syndrome among twins is related to high fat Western diet. A diet with fewer vegetables is correlated with Crohn’s inflammatory bowel disease. These patients have less AhRs and altered IL-22. If AhRs were present, they showed much stronger immune response. It is not yet known whether fruits and vegetables are the major factors stimulating AhRs, but they seem to be. This could well be the mechanism that allows fruits and vegetables to help the ability of the intestine epithelial cells to keep microbes out.
Signaling Cascades from Micronutrients Meet and Interact in the Nucleus
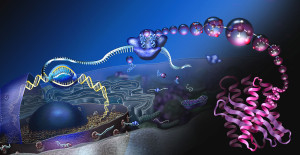 All of these active ingredients—vitamins and other micronutrients from food—have cascades of molecules that meet in the nucleus. The interactions between them are extremely complex and just being discovered. They involve the receptors that trigger cascades to the nucleus and, also, special receptors in the nucleus itself. They all interact in extremely complex ways to trigger genetic networks and immune functions. Vitamin D and A are known to be part of this with their own nuclear receptors receptors.
All of these active ingredients—vitamins and other micronutrients from food—have cascades of molecules that meet in the nucleus. The interactions between them are extremely complex and just being discovered. They involve the receptors that trigger cascades to the nucleus and, also, special receptors in the nucleus itself. They all interact in extremely complex ways to trigger genetic networks and immune functions. Vitamin D and A are known to be part of this with their own nuclear receptors receptors.
Nutrients are taken in by the intestinal epithelial cells and sent in the blood. Some are altered in the in the liver and kidneys to become important active molecules. The nutrients enter the cells and stimulate receptors inside, which travel to the nucleus, which along with many other factors stimulate genetic networks. Vitamin A binds to the retinoic acid receptor (RAR) and forms the complex retinoic X receptor RXR. This receptor is in the nucleus and affects how retinoids stimulate genetic networks. Each of these have many forms and subunits. These nuclear receptors are varied in different kinds of cells and produce a variety of “response elements” (RAREs).
 Vitamin D from skin that has been modified by the sun goes to the liver and kidney creating active molecules (especially 1,25-(OH)2D3), which stimulate vitamin D receptor (VDR) and complexes with RXR making the vitamin D response elements (VDREs).
Vitamin D from skin that has been modified by the sun goes to the liver and kidney creating active molecules (especially 1,25-(OH)2D3), which stimulate vitamin D receptor (VDR) and complexes with RXR making the vitamin D response elements (VDREs).
Arylhydrocarbons, such as DIM from food and microbes stimulate the AhR receptors. These cascade to the nucleus making other response elements (XREs). Arylhydrocarbons include molecules from plants such as flavonoids, plypheolics, and indoles. They include man made molecules such as synthetic polycyclic aromatic hydrocarbons and substances like dioxin.
All of these receptors utilize very complex nuclear mechanisms involving epigenetic histone tags, transcription factors and many different DNA activators and repressors.
Vitamin D and Immune Cells
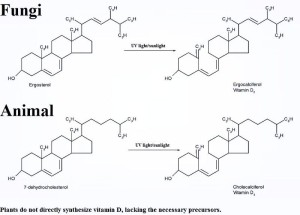
Vitamin D is uniquely critical for intestinal lymphocytes (IELs), which are maintained on a daily basis by them. Vitamin D influences the thymus (the center of the T cell development – the critical organizer of the immune system). Vitamin D3 (the active ingredient) interacts closely with Vitamin A in the nucleus. It is critical for the IELs of the intestinal lining and the maintenance of control of the microbes there.
Vitamin D is actually an entire group of different molecules called calciferols, which come from diet in small amount and skin cells stimulated by the sun in larger amount, metabolized from cholesterol. Both D2 and D3 come from food and the distinction between them is not yet totally clear. Animals bring 25 hydroxyvitamin D3. This is inactive and has to be altered (as vitamin A) in the liver and kidney. Also, immune cells can make these active metabolites. Calcitriol, from D3, is the active molecule. D2, or ergocalciferol, is processed to 25-hydroxyergocalciferol. Immune dendritic cells and macrophages have the enzymes to do this, but how they make it is not clear. It is not enough to help the immune cells at the skin. Vitamin D metabolism has critical effects on calcium and phosphorus metabolism and bone. Many people do not have enough Vitamin D in the winter.
Inflammation, Vitamin D and Vitamin A
Inflammatory bowel diseases (IBD) are affected by genes (30%) and environment. Both microbes and nutrients play a big role. Both vitamin D and A are important. Without enough vitamin D people can develop asthma, diabetes, autoimmunity and infections. These produce altered T cell activity. There are many different types of T cells that are produced in different circumstances at the skin and intestine. The complex T regulatory cells are produced locally for special conditions and respond to a wide variety of cytokines from human cells and microbes.
Short chain fatty acids from diet (butyrate) are critical for the development of these special T cells. They are clearly related to specific dietary factors, but the research is very complex and not well understood at this moment.
Diet affects health in every way, both stimulating healthy responses and causing disease (obesity, heart disease, cancer and diabetes). These nutrients affect immune cells in complex ways including the development of the critical lymph tissues that create the wide variety of different cells. Microbe products are, also, critical and influence micronutrients and at the same time, microbes are influenced by the diet.
Special types of microbes exist with different diets. Recently, it was found that eating red meat attracts particular microbes that like to eat the meat’s carnitine, which creates a byproduct. This byproduct is absorbed and changed into a substance that produces plaque and clots in the blood vessels causing heart disease. Vegetarians have different kinds of microbes. (See post Five Secrets of Brain Health). One problem with the complexity of this research is the unique responses in the human gut from other research animals.
How Does Diet Influence Immunity
 The extremely complex ways that ingested foods and products made by microbes affect our immunity is just being discovered. The intelligent signaling of epithelial structural cells at the barriers of skin and gut determine the outcome of immune function. These cells make a vast amount of decisions about friendly and non-friendly microbes, as well as calling for and training the exact immune cells that are needed. Through signaling they inform the immune cells whether to react or not to situations and how to build the specialized lymph nodes that deal with unique types of inflammation.They, also, make decisions about digestion.
The extremely complex ways that ingested foods and products made by microbes affect our immunity is just being discovered. The intelligent signaling of epithelial structural cells at the barriers of skin and gut determine the outcome of immune function. These cells make a vast amount of decisions about friendly and non-friendly microbes, as well as calling for and training the exact immune cells that are needed. Through signaling they inform the immune cells whether to react or not to situations and how to build the specialized lymph nodes that deal with unique types of inflammation.They, also, make decisions about digestion.
This back and forth communication is very elaborate. Is it possible to think that these processes are random? How can anyone not see the incredible intelligent work and decision making being done by this one layer of cells? This intelligent communication and decision making between cells is vital for our function at every level?