Placebos can influence health outcomes, but, it has not been clear how this happens. Recent posts have described how mental activity, such as expectations, determine perception, rather than just physical sensory information. Now, placebos demonstrate that perception alters physical health. Research shows that diverse brain regions are involved, including stimulation of natural opiod neurotransmitters and dopamine. Most of the research addressing these mechanisms has been related to placebo affects on pain, which have been the easiest to study.
Placebos can influence health outcomes, but, it has not been clear how this happens. Recent posts have described how mental activity, such as expectations, determine perception, rather than just physical sensory information. Now, placebos demonstrate that perception alters physical health. Research shows that diverse brain regions are involved, including stimulation of natural opiod neurotransmitters and dopamine. Most of the research addressing these mechanisms has been related to placebo affects on pain, which have been the easiest to study.

Placebos work through the effects of clinical rituals, symbols and interactions with health care. The manner and explanations of doctors and other health care providers are major aspects of the effect.
It has long been noted that the way doctors, therapists and nurses treat patients have dramatic effects on whether patients improve or not. The study of placebos has documented the details of the brain reactions for this therapeutic response.

In the very busy world of increasingly high technology medicine, the importance of how clinicians treat patients is being obscured. Some of the old words for the positive effects of placebos, are “laying on of hands,” empathy and listening, which have positive therapeutic effects. The science of placebos is re opening this important area of the clinician’s approach, and will have implications for the future function of doctors, even while the rush to computerize takes the doctor’s eyes off of the patient and onto a computer screen. Placebo affects in the brain will map the way concepts alter physical states.
Placebos and Pain
Pain and the distresses caused by illness have been difficult to treat, as are depression and chronic fatigue. Illnesses that triggers pain, fatigue and depression are especially complex because they involve brain circuits not just bodily organs. Understanding these processes involves study of subjective experience, which is not measurable. Also, as many previous posts have noted, there is no brain region for subjective experience.
By definition, placebos don’t have physiological or therapeutic effects. But, in fact, studies show that in many cases the way that a doctor or therapist interacts with a patient can have therapeutic (placebo) or negative (nocebo) affects on symptoms. The type of interaction becomes highly connected with expectations, emotions and memories that can have great impact on physiological processes. Previous posts show that even visual perceptions are determined as much by expectations as by the incoming sensory data.
It is not known to what extent treatment outcomes depend on the therapeutic context rather than the specific surgery, medication or lifestyle changes. Drug trials, today, are almost always compared to placebos and there is usually a definite percent of improvement with the placebo group—as much as thirty or forty percent in some trials. In general, as society is more aware of drug trials the placebo response in medication trials has increased over time. Some have tried to not count the placebo groups in medication trials, but they may be the ones who may have an even better effect with the real medication.
There are a variety of different cues that can have impact on symptoms. The presentation of the doctors office, the white coat, the manner of interaction of the doctor—how confident she is—and suggestions that the patient will improve. Previous reactions to clinical settings can have a negative impact as well. Other factors are how expectations of treatment are set. All of these social and context cues have brain effects.
Placebo Effects in Disease
The question of what is a “real” symptom is often used to rationalize views against the importance of placebo effects. This view is that if the placebo helps then the symptom wasn’t real to begin with. But, there is much evidence that placebos can have definite physiological effects including altering hormones, the neurological autonomic responses, the immune system, and behavior.
Studies show effectiveness of placebos in Parkinson’s disease, asthma, chronic pain and depression. They have helped lower mortality in cardiovascular diseases. All of these involve the patient’s knowing that they are receiving treatment. Some who are on placebo may also have a med card for medical marijuana to help them with their pain, this may have to be stopped when they are doing their placebo treatment, it is up to the doctors who are conducting the treatment.
One study gave people three different placebo creams and they were told that each had different strengths. The three different levels of placebo creams reduced experimental applied pain in the same three levels. The control group and weak placebo had little effect. The “strongest” cream had a marked effect in reducing the pain. Measurements were, also, made of pupil diameters, vital signs and EEGs, which, also showed gradual lessening of pain reactions over several applications. More trials further reduced the measured pain effects.
When a negative suggestion was given that pain will increase, cortisol levels increased. In another experiment an injected medication was given repeatedly that increased cortisol and growth hormone. When saline injection was later given it had the same effect because of the expectation.
Two identical milkshakes, one labeled “indulgent” and the other “sensible” were given. The “indulgent” drink reduced a hormone (ghrelin) that increases appetite, while the other didn’t.

A particular flavored drink was given to both mice and humans at the same time as a drug that decreases immune response (cyclosporine A). Later, in both mice and humans, just taking the drink (and not the cyclosporine A) produced the same immune response. The response involved the amount of T cells and levels of interleukin-2 and interferon-?. There is some evidence that this is related to forebrain norepinephrine circuits.
Another study showed a decrease of skin reaction to an allergen with a placebo. Headaches caused by high altitude were helped by a placebo that affected levels of prostaglandin. This study included communication about the expectation of effect by the placebo to one person who told it to another who, then, had the positive placebo response. It demonstrated the influence of a social network of information.
Complexity of Pain and Placebo
One criticism of placebo effects on pain is that pain is completely subjective and the response could be created by a different attitude toward the pain. Changes in attitudes are part of cognitive therapies helping pain. Also, meditation studies of the brain show that with extensive meditation (see post) there is more awareness of the pain, but less actual painful feeling—a version of a different vantage point of evaluation. Other types of bias including reporting more pain to get more attention and having less pain to please the researcher.
Also, effects can be from subjective attitudes that change people’s lifestyle including what they eat, what medications they will take.
Brain Imaging

Spinal nociceptive circuits are active during pain. This includes medial thalamus, primary and secondary somatosensory cortex (S1 and S2), dorsal posterior, mid and anterior insula and the dorsal anterior cingulate cortex. These circuits have less activity with placebo, particularly the thalamus, cingulate cortex and insula, even with pain stimuli. The improvements occurred with laser stimuli demonstrating rapid responses.
Inclusion of emotions and decision-making in our experience of pain complicates the study of pain. The regions mentioned above are, also, involved in decision making of other issues and emotional responses unrelated to pain. The insula and S2 are the most purely related to physical pain. There are variable responses to different individuals, studies and methods of pain production.
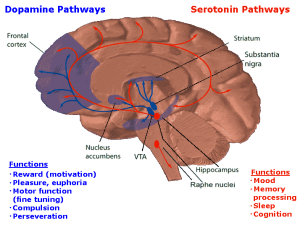 Other influential circuits modulating pain come from the brainstem, involving neurotransmitters serotonin and norepinephrine, but, also, dopamine, opiods, cholecystokinin and neurokinin1. These circuits block pain effects at the dorsal horn of the spinal cord. Placebos can, also, provide this same relief.
Other influential circuits modulating pain come from the brainstem, involving neurotransmitters serotonin and norepinephrine, but, also, dopamine, opiods, cholecystokinin and neurokinin1. These circuits block pain effects at the dorsal horn of the spinal cord. Placebos can, also, provide this same relief.
The periaqueductal gray region (PAG) is highly related to pain and sends fibers to the medulla and the spinal cord. It receives communication from many critical brain regions in the prefrontal cortex, amygdala, hypothalamus and the nucleus accumbens (see post on pleasure circuits in the brain for detailed description of the nucleus accumbens.) These circuits modulate pain from centers of emotion, motivation and decision-making.
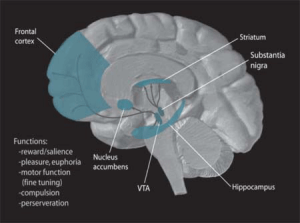 Placebos causing decrease of pain are blocked by medication naloxone the blocks opiods pathways. PET imaging shows increased ?-opiods in the PAG during placebo response to pain. Also, fMRI BOLD activity in the PAG show decreased pain activity with placebos. The PAG effects on decreasing pain are inhibited by naloxone.
Placebos causing decrease of pain are blocked by medication naloxone the blocks opiods pathways. PET imaging shows increased ?-opiods in the PAG during placebo response to pain. Also, fMRI BOLD activity in the PAG show decreased pain activity with placebos. The PAG effects on decreasing pain are inhibited by naloxone.
Suggestions of increased pain (nocebo) can increase imaging activity to pain, blocking analgesia. This occurs through the spinal pathways of the emotional centers. There is evidence of increased activity through the higher centers during pain and nocebo effects. In fact, placebos affect many areas of the higher regions of the cortex and they correlate with the amount of analgesia. These include thinking about the pain before and afterward.
Transcranial stimulation of parts of the pre frontal cortex at particular frequencies can decrease or increase pain. These, also, involve the PAG. Placebos appear to increase the activity between the prefrontal cortex and the PAG. This increase in activity is blocked by naloxone—meaning that opiod transmission in the higher brain regions are involved with the placebo response.
In animal studies, the activity between pre frontal cortex and PAG are important to modulate pain. If the PFC is stimulated in the lateral orbital region then the PAG secretes opiates to block the pain.
 Placebos increase activity in nucleus accumbens and decreases amygdala activity increasing secretion of opiods. The amygdala is involved in threats and fearfulness and these are decreased with placebo triggering of opiods. The amygdala is important in both regular pain and placebo reactions to pain.
Placebos increase activity in nucleus accumbens and decreases amygdala activity increasing secretion of opiods. The amygdala is involved in threats and fearfulness and these are decreased with placebo triggering of opiods. The amygdala is important in both regular pain and placebo reactions to pain.
The nucleus accumbens is noted to be very complex (see post on pleasure response in the brain) and recent research finds very specific hubs that both increase and decrease a variety of emotions. Placebos increase opiod and dopamine responses. The circuit between nucleus accumbens and the ventro medial pre frontal cortex is highly related to long-term pain behavior. These circuits may predict who will respond to a placebo.
Motivation and Placebos
PET study showed placebo stimulated more dopamine in striatum in Parkinson’s patient demonstrating increased movement and motivation. This increase of dopamine affected the reward learning activity in the striatum and pre frontal cortex, as well.
Placebo lowered the activity in the brain hub subgenual cingulate cortex, which is correlated with depression. Similar affects occurred for anxiety with changes in the cortex. Giving a placebo for “nausea” decreased the sense of disgust.
Summary: Placebos stimulate cortical and subcortical circuits related to expectation, and emotions. They stimulate the circuits that modulate pain signals in the spinal cord and the emotional and motivation circuits in the amygdala, cortex and striatum. The brainstem stimulates opiods, and other neurotransmitters, and can be blocked by naloxone. Oxytocin increased placebo pain reduction.
Mechanisms of Placebo in the Brain
Placebo effects include sensory clues, unconscious and conscious expectations.
- Positive sensory cues that predict a positive or negative result from the placebo, including setting and types of suggestions.
 Some expectations and results are based on unconscious pre conceptions independent from conscious ideas and beliefs that might relate to the placebo effect. These can be conditioned responses, such as associations of an event with pre existing response. These are unconscious memories that have had neuroplastic circuits.
Some expectations and results are based on unconscious pre conceptions independent from conscious ideas and beliefs that might relate to the placebo effect. These can be conditioned responses, such as associations of an event with pre existing response. These are unconscious memories that have had neuroplastic circuits.- The other stimuli are conscious attitudes, beliefs, memories and expectations related to the problem and the treatments.
- If these are strong, then emotional reactions may be triggered.
- All three can have different effects in different brain circuits.
It is not clear if the same circuits are involved in the different outcomes involving pain versus depression and Parkinson’s. Some studies show a combined effect on pain and negative emotional responses. Most studies have used both conscious suggestions as well as conditioned stimuli. There has been no way to separate placebo mechanisms related to belief in the effect of the placebo, positive expectations and through conditioned learning. All might be involved at the same time. If a patient is told that a strong pain is coming, then both the reinforcement and emotions are involved in the cortisol response. In some cases verbal suggestions can alter conditioning—for example, stating that the previous shock associated with an event is not longer active. There are probably too many individual differences to make sense at our current level of circuit understanding. If we take a pain pill and the pain stops, is it the pill or the expectation?
It is surprising that placebo effects may increase over time, despite continued pain or other symptoms.
Clinical Care
 The circuits involved with placebos are, also, affected by medications. Placebos are noted to help symptoms but not cure illnesses. The diseases are not substantially altered but rather subjective symptoms of pain, anxiety, and depression are altered. Behavior can be altered including movement problems in Parkinson’s, which has strong affective components.
The circuits involved with placebos are, also, affected by medications. Placebos are noted to help symptoms but not cure illnesses. The diseases are not substantially altered but rather subjective symptoms of pain, anxiety, and depression are altered. Behavior can be altered including movement problems in Parkinson’s, which has strong affective components.
Placebos don’t eliminate tumors, but help nausea, fatigue and pain. In asthma, they don’t affect the underlying lung pathology but help symptoms of shortness of breath.
One study with migraine medication, found that if the real medication was called a placebo, the results were the same as a placebo. If the tablet was properly marked it was 50% more effective. Similar effects occur with pain medications.
Nocebo effects occur when people are worried about side effects. Many of these effects appear upon reading about the medication. In fact, “medical student’s disease” occurs in young training doctors reading about symptoms—they develop some of the symptoms. When told of sexual side effects from a medication, patients had three times the effect as if not told. This makes ethical decisions difficult for doctors in a modern internet world where every one wants to know all the possible side effects, even if they are very rare.
Placebos cause different side effects than the regular medication, as well. A percentage of patients treated with placebos stop taking the medication because of side effects that are unrelated to anything the medication might cause.
A recent perspective in the New England Journal of Medicine raises the questions of the best ways for doctors to deal with the effects of placebos in clinical practice (Placebo Effects in Medicine, Ted J. Kaptchuk and Franklin G. Miller, Ph.D., July 2, 2015). With pressure for doctors to be completely transparent with patients today, it is not clear what the best approach should be—that is, to provide the positive placebo effects, while avoiding the negative nocebo effects and being completely direct. Recently, study is being undertaken concerning telling patients that they are taking a placebo for a real illness.
Placebo Affects In the Brain
It is impossible to separate the mind and the body. Physical illness greatly affects the mind and mental states greatly affect physical symptoms. Both exist together in a continuum. Hopefully, as the relation of mind to creatures, organs, cells and chemicals becomes clearer, the relationship can be used for benefit.
Mental events trigger events in brain circuits, individual neurons, microtubule and actin scaffolding, and genetic networks. Specific mental concepts trigger placebo effects that trigger varied neuro endocrine effects. Studies of the placebo, like studies of conscious mental activity in meditation, have important lessons in how mind operates with molecules in nature. Perception alters physical health.