 The skin is the major interface between the body and the outside world with its trillions of microbes and environmental toxins. Skin has many layers and various different types of cells—keratinocytes, fibroblasts that make the extra cellular matrix, immune cells of various types, and sensory cells that connect to nerve fibers. The most important cell—and most numerous—is the keratinocyte, which undergoes modifications in each layer and has extensive conversations with immune cells, connective tissue cells and microbes. The skin is second only to the gut in the amount of microbes that it encounters. A previous post about the intelligent intestinal epithelial cell showed that one layer of cells communicates with 100 trillion friendly and unfriendly microbes in the lumen, as well as, many immune cells below. The complex back and forth communication determines digestion and gives critical immune direction to the entire body. The skin is, also, a very complex community of cells that ensures immune defense against dangerous intruders and injuries and maintains the stability of its surface to the outside world. The very intelligent skin cell directs this activity by engaging in critical complex back and forth communication with many other cells.
The skin is the major interface between the body and the outside world with its trillions of microbes and environmental toxins. Skin has many layers and various different types of cells—keratinocytes, fibroblasts that make the extra cellular matrix, immune cells of various types, and sensory cells that connect to nerve fibers. The most important cell—and most numerous—is the keratinocyte, which undergoes modifications in each layer and has extensive conversations with immune cells, connective tissue cells and microbes. The skin is second only to the gut in the amount of microbes that it encounters. A previous post about the intelligent intestinal epithelial cell showed that one layer of cells communicates with 100 trillion friendly and unfriendly microbes in the lumen, as well as, many immune cells below. The complex back and forth communication determines digestion and gives critical immune direction to the entire body. The skin is, also, a very complex community of cells that ensures immune defense against dangerous intruders and injuries and maintains the stability of its surface to the outside world. The very intelligent skin cell directs this activity by engaging in critical complex back and forth communication with many other cells.
 The skin provides mechanical barriers, which decreases the loss of water and avoids the uptake of toxins and microbes. The skin is, also, a critical center of immune activity; it is a first line of defense with structural barriers in connective tissue and stromal cells. The skin has many different specific immune cells that fulfill a wide range of jobs in different situations. Just as in the intestine, it is the complex cross talk between these cells that determines the growth and maintenance of the immune tissues below. This cross talk is critical in maintaining skin’s structure in the face of injuries, cuts and infections. Just as the intestine, there are a large amount of friendly microbe communities that live near the skin and influence the local and total body immune function. It is back and forth molecular communication that determines the critical friendly microbes that are allowed to stay on the surface.
The skin provides mechanical barriers, which decreases the loss of water and avoids the uptake of toxins and microbes. The skin is, also, a critical center of immune activity; it is a first line of defense with structural barriers in connective tissue and stromal cells. The skin has many different specific immune cells that fulfill a wide range of jobs in different situations. Just as in the intestine, it is the complex cross talk between these cells that determines the growth and maintenance of the immune tissues below. This cross talk is critical in maintaining skin’s structure in the face of injuries, cuts and infections. Just as the intestine, there are a large amount of friendly microbe communities that live near the skin and influence the local and total body immune function. It is back and forth molecular communication that determines the critical friendly microbes that are allowed to stay on the surface.
Previously, the study of immunity focused on immune cells. Now, it is understood that a complex back and forth communication between epithelial, connective tissue cells and immune cells determines all of the activity.
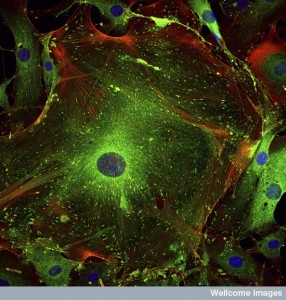
Epithelial Cells – Keratinocytes
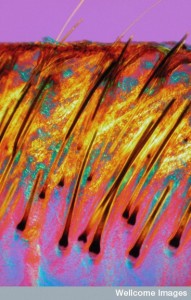 Epithelial cells exist in the hair follicle and in between the follicles—the most common is the keratinocyte, which undergoes a gradual differentiation to a surface cell that doesn’t have a nucleus. Keratinocytes protect nerves, providing tight junctions, and they hold the immune Langherhans cells and T cells in place in the epidermis. They are extremely active in directing the activity of the skin through extensive signaling.
Epithelial cells exist in the hair follicle and in between the follicles—the most common is the keratinocyte, which undergoes a gradual differentiation to a surface cell that doesn’t have a nucleus. Keratinocytes protect nerves, providing tight junctions, and they hold the immune Langherhans cells and T cells in place in the epidermis. They are extremely active in directing the activity of the skin through extensive signaling.
Keratinocytes receive messages from microbes and the environment and alert the structural fibroblasts and immune cells of what they must provide. Keratinocytes have many receptors that sense microbes and stress factors. They frequently use a wide variety of cytokine signals, including many from large prominent cytokine families—IL-1, Il-10, Il-20 and TNF. They initiate signals to start and stop inflammation. There are critical transcription factors in keratinocytes, (such as JUN and FOS), that affect networks of genes and turn on programs to start and stop inflammation. In people with psoriasis, there is less JUN in the skin cells allowing inflammation and arthritis. The keratinocyte signals can by themselves activate some inflammatory skin diseases.
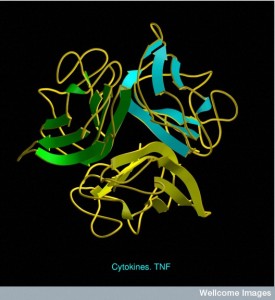 In many skin diseases the keratinocytes have specific factors that trigger networks of genes that then call for very specific types of immune cells (among possibly hundreds of subtypes). There are a wide variety of very complex signals from the keratinocytes that mediate skin reactions in many situations. Specific immune cells are called to the skin (by chemokine signals) and start the inflammatory process (with cytokines). Mast cells, macrophages, dendritic cells, T cells, and γδ cells, all have subtypes that are specific to the skin and called up through a very detailed cytokine language.
In many skin diseases the keratinocytes have specific factors that trigger networks of genes that then call for very specific types of immune cells (among possibly hundreds of subtypes). There are a wide variety of very complex signals from the keratinocytes that mediate skin reactions in many situations. Specific immune cells are called to the skin (by chemokine signals) and start the inflammatory process (with cytokines). Mast cells, macrophages, dendritic cells, T cells, and γδ cells, all have subtypes that are specific to the skin and called up through a very detailed cytokine language.
When a keratinocyte dies, it provides a strong stimulation of skin inflammation by releasing molecules that are damage associated molecular patterns (DAMPs), which activate immune cell receptors and trigger inflammation.
In some cases keratinocytes deliberately kill themselves to produce this effect (through apoptosis-programmed cell death pathways). Apoptosis is a critical pathway to communicate the need to trigger inflammation in both skin and gut—the two great barrier regions. Apoptosis pathways are dependent upon TNF cytokine pathways. Many different bacteria and viruses have the ability to inhibit some of the TNF pathways, and can control some of the reactions of keratinocytes.
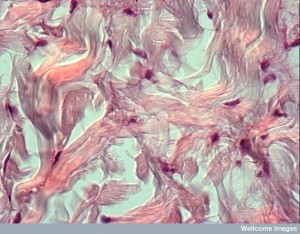
Connective Tissue Cells
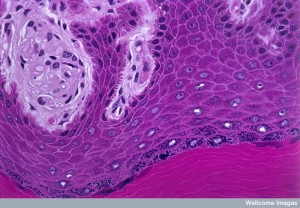
 Fibroblasts secrete connective tissue and extracellular matrix, which maintains the barrier and aids in injury repair. Fibroblasts, also, engage in the critical back and forth communication with keratinocytes. This extracellular matrix exists between the two layers of skin—dermis and epidermis. In the epidermis, the keratinocytes live on the elaborate scaffold of this matrix laid down by fibroblasts. Even extra cellular material takes part in the communication (see post ECM) Fixed in this matrix the cells join together at the top skin layer. The connective tissue is made up of fibers, cells and ground substance. All the cells are spread out in extracellular fluid. The ground substance is a thick fluid with glycoaminoglycans and proteoglycans. Microbes have a hard time making it through the viscous ground substance. Fat cells are also kept in place by collagen fibers and allow a cushion.
Fibroblasts secrete connective tissue and extracellular matrix, which maintains the barrier and aids in injury repair. Fibroblasts, also, engage in the critical back and forth communication with keratinocytes. This extracellular matrix exists between the two layers of skin—dermis and epidermis. In the epidermis, the keratinocytes live on the elaborate scaffold of this matrix laid down by fibroblasts. Even extra cellular material takes part in the communication (see post ECM) Fixed in this matrix the cells join together at the top skin layer. The connective tissue is made up of fibers, cells and ground substance. All the cells are spread out in extracellular fluid. The ground substance is a thick fluid with glycoaminoglycans and proteoglycans. Microbes have a hard time making it through the viscous ground substance. Fat cells are also kept in place by collagen fibers and allow a cushion.
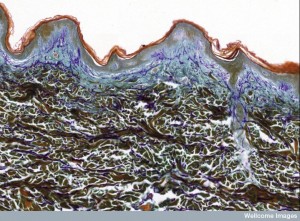
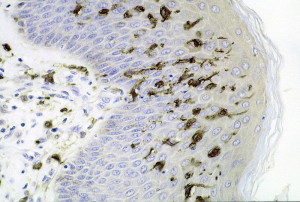
Epidermis – The Top Layer
 The skin is made of epidermis and dermis. The epidermis has keratinocytes that are proliferating and some that are fully differentiated. Epidermis is the major barrier against toxins, microbes and infection and regulates water release. It varies in size from 0.002 inches in eyelids to 0.06 inches in palms and soles. There are no blood vessels in epidermis and oxygen diffuses from the air to nourish the cells. 95% of the cells are keratinocytes along with some melanocytes, immune cells called Langerhans cells, other travelling immune cells, and Merkel cells (oval receptor cells that connect with sensory fibers). Beneath the epidermis there is a layer of blood capillaries.
The skin is made of epidermis and dermis. The epidermis has keratinocytes that are proliferating and some that are fully differentiated. Epidermis is the major barrier against toxins, microbes and infection and regulates water release. It varies in size from 0.002 inches in eyelids to 0.06 inches in palms and soles. There are no blood vessels in epidermis and oxygen diffuses from the air to nourish the cells. 95% of the cells are keratinocytes along with some melanocytes, immune cells called Langerhans cells, other travelling immune cells, and Merkel cells (oval receptor cells that connect with sensory fibers). Beneath the epidermis there is a layer of blood capillaries.
The epidermis forms a physical barrier with very tight cell-to-cell junctions and many structural proteins. It is a chemical barrier with lipids, acids, enzymes and antimicrobial peptides. It is, also, an immune barrier. The surface has water and acid pH making it harder for microbes.
Epidermis is made of four layers
 The bottom basal layer is where stem cells make more keratinocytes that can either divide or travel and differentiate. Some of the new keratinocytes rise to the other layers. Basal cells are attached to a basement membrane. Melanocytes are in this basal layer making melanin in a vesicle, which is moved along arms (called dendrites) that connect with the keratinocytes. Melanin becomes a cover for the nucleus of the keratinocyte. The Merkel receptors that link to sensory fibers are also in this level, especially in the fingertips.
The bottom basal layer is where stem cells make more keratinocytes that can either divide or travel and differentiate. Some of the new keratinocytes rise to the other layers. Basal cells are attached to a basement membrane. Melanocytes are in this basal layer making melanin in a vesicle, which is moved along arms (called dendrites) that connect with the keratinocytes. Melanin becomes a cover for the nucleus of the keratinocyte. The Merkel receptors that link to sensory fibers are also in this level, especially in the fingertips.- The next layer up has keratinocytes connected with an elaborate tight junction adhesion structure. Langerhans immune cells live in the middle of this layer.
 The third granular layer is where keratinocytes start to lose their nuclei. It has a large lipid barrier made of material released from the keratinocytes. The lipids become non polar and are placed parallel to the surface (ceramides and free fatty acids).
The third granular layer is where keratinocytes start to lose their nuclei. It has a large lipid barrier made of material released from the keratinocytes. The lipids become non polar and are placed parallel to the surface (ceramides and free fatty acids).- The top hard level consists of 20 layers of keratinocytes that have lost their nuclei through differentiation (corneocytes are the final differentiated keratinocytes.) These are surrounded by water retaining proteins and fat cells.
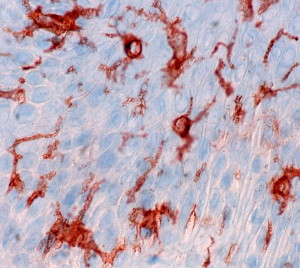
Dermis – The Layer Below Basement Membrane
 The dermis is below and connected tightly by the basement membrane. The dermis is made up of many fibers providing an elaborate extracellular matrix of collagen (for strength) and elastin (for elasticity). In addition there is another extra-fibrillary matrix—a gel made of glyocoaminoglycans, proteoglycans and glycoproteins. In it there are receptors that sense mechanical forces including touch and heat. It includes hair follicles; sweat, sebaceous and apocrine glands; and lymph and blood vessels. These vessels nourish and remove waste from both layers. The major cells are fibroblasts, macrophages and fat cells.
The dermis is below and connected tightly by the basement membrane. The dermis is made up of many fibers providing an elaborate extracellular matrix of collagen (for strength) and elastin (for elasticity). In addition there is another extra-fibrillary matrix—a gel made of glyocoaminoglycans, proteoglycans and glycoproteins. In it there are receptors that sense mechanical forces including touch and heat. It includes hair follicles; sweat, sebaceous and apocrine glands; and lymph and blood vessels. These vessels nourish and remove waste from both layers. The major cells are fibroblasts, macrophages and fat cells.
The skin has a very active extra cellular matrix, ECM (see post on Extra cellular matrix). The structural cellular elements that produce the ECM are stromal cells, (connective tissue) such as fibroblasts, as well as, the epithelial cells that form the blood and lymph vessels. This extracellular matrix is also active in communication with keratinocytes concerning immunity.
Immune Cells in Skin
 The skin has many interspersed immune cells such as Langherhans cells and dendritic epidermal T cells (DETCs). These immune cells, along with many other’s that are recruited from a distance when trouble occurs, are specific for the skin. Langherhans cells are immune cells specific to the skin that pick up microbes and antigens and present them to the T cells.
The skin has many interspersed immune cells such as Langherhans cells and dendritic epidermal T cells (DETCs). These immune cells, along with many other’s that are recruited from a distance when trouble occurs, are specific for the skin. Langherhans cells are immune cells specific to the skin that pick up microbes and antigens and present them to the T cells.
As well as permanent immune cells in the skin, a variety of cells, also, travel through. Some of these cells are born in bone marrow and travel to the skin by way of the blood vessels and some are created in the liver or yolk sac. Cells originally formed elsewhere, can renew and produce new cells in the skin tissues.
Signals from the keratinocytes in a troubled region alert the system that more immune cells are needed in a particular area. Keratinocytes send several signals (IL-34), which are needed to allow more Langherhans cells in the region. During inflammation and stress, the keratinocytes at the hair follicles are the cells that send chemokines CCL2, CCL20 to attract Langherhans, or CCL8 to stop them. The hair follicles are critical points of entry of these immune cells that are being recruited.
 There are subsets of antigen-producing cells that use a wide variety of other signals. These specific cells promote certain T cells (such as T helper 17) when particular microbes are present. The Langherhans cells, also, provide a controlling effect, which can reduce the activity of the T cells. These signals control whether immune cells will turn against the organism and cause autoimmune disease. Thus, Langerhans cells can fight against inflammation or promote it.
There are subsets of antigen-producing cells that use a wide variety of other signals. These specific cells promote certain T cells (such as T helper 17) when particular microbes are present. The Langherhans cells, also, provide a controlling effect, which can reduce the activity of the T cells. These signals control whether immune cells will turn against the organism and cause autoimmune disease. Thus, Langerhans cells can fight against inflammation or promote it.
Different types of skin inflammation attract different types of immune cells through elaborate signaling. It is the keratinocyte that calls for these different types of immune cells (in psoriasis and atopic dermatitis for example.) Entirely different types of cells are signaled in different virus infections. With lupus skin lesions, other types of cells are produced and inhibited.
 Some of the cells that are attracted are macrophages and monocytes. These cells survey the tissue looking for microbes and then help get pieces of the microbes to the draining lymph nodes where T cells can find them and create a reaction to come and kill them. They can contribute to inflammation to fight a microbe infection, help regulate the battle, and heal the wound afterward.
Some of the cells that are attracted are macrophages and monocytes. These cells survey the tissue looking for microbes and then help get pieces of the microbes to the draining lymph nodes where T cells can find them and create a reaction to come and kill them. They can contribute to inflammation to fight a microbe infection, help regulate the battle, and heal the wound afterward.
The different types of cells are formed based on the complex cross talk with the keratinocytes. One example is when macrophages, under the influence of communication, form special subtypes that provide the unique required functions.
Another cell, the mast cell, has many roles with specific microbes in the skin. Mast cells, as well as other immune cells, can increase inflammation to kill microbes, as well as, the opposite anti inflammatory cleanup role.
Local T cells are able to start an inflammation without circulating cells. In fact, there are 1010 T cells in the skin, which is double the number of T cells circulating in the blood and lymph. It is the resident T cells that are better able to fight herpes. Other studies have shown that memory T cells in the skin provide the necessary protection for further infection.
Another special immune cell, called γδ, leaves thymus tissue, travels to the skin and specially watches for cancer cells, as well as, other infections and skin diseases.
Microbes Communicate Back and Forth with Skin Cells
 The skin has a very large number of microbe communities with which it interacts, like the other great barrier—the intestinal epithelial cell. The microbes send signals to the keratinocytes, to the extracellular matrix and to immune cells to establish friendly relations. Very particular microbe communities are allowed to live in specific places on the skin. These friendly microbes help repel dangerous microbes on the skin, as is done in the gut. This communication can benefit the skin cells or turn against them.
The skin has a very large number of microbe communities with which it interacts, like the other great barrier—the intestinal epithelial cell. The microbes send signals to the keratinocytes, to the extracellular matrix and to immune cells to establish friendly relations. Very particular microbe communities are allowed to live in specific places on the skin. These friendly microbes help repel dangerous microbes on the skin, as is done in the gut. This communication can benefit the skin cells or turn against them.
Keratinocytes and microbes keep up an elaborate back and forth conversation. The keratinocytes send different specific peptides (much as the Paneth cells do in the intestine). These peptides control the growth and the types of microbes that are allowed near the skin. The immune cells also release specific peptides for friendly and enemy microbes, as well as communicating with the skin cells. But, these immune messages from T cells, B cells, Langerhans cells are not nearly as important as the messages from the keratinocytes. The immune cells most importantly must communicate through the skin cells.
Keratinocytes maintain the normal situation and are critical in triggering inflammation. In order to have effective immunity at the skin, the keratinocytes must allow colonization of specific microbes that then become essential for appropriate T cell responses later. Research shows that germ free skin does not have effective T cell responses when danger arises. When friendly microbes are allowed to colonize the skin, the T cell response became effective again. Both the keratinocyte allowing colonization, as well as, communication with keratinocytes are essential.
When some specific dangerous bacteria are able to colonize the skin, there are specific pathological immune responses and inflammation. These microbes are able to directly affect the immune cells and circumvent the effects of the keratinocytes.
 The elaborate cross talk, also, includes the connective cells and their fibers. These fibroblasts, also, send communication signals to the keratinocytes and the microbes. Fibroblasts create the connective tissue and extra cellular barriers that can be specific to certain microbes.
The elaborate cross talk, also, includes the connective cells and their fibers. These fibroblasts, also, send communication signals to the keratinocytes and the microbes. Fibroblasts create the connective tissue and extra cellular barriers that can be specific to certain microbes.
The elaborate conversation includes the many different keratinocytes, fibroblasts, immune cells and microbes.
The Very Intelligent Skin Cell
Increasingly, it is found that cells use elaborate communication to accomplish all types of physiological functions. Because of the critical barrier function of skin cells and intestinal epithelial cells, they direct these efforts by using very complex elaborate communication with many cells—epithelial cells, connective cells, extra cellular matrix, many different microbes, and many different immune cells. In fact, the types of immune cells are chosen among hundreds of possibilities for the exact situation and microbe invader.
 The keratinocytes are not at all passive cells, but extremely active in determining both the types of microbes that are allowed near the skin and in calling for the very specific immune cells that are necessary to deal with many different situations. In this elaborate cross talk, hundreds of different cytokines and chemokines (attracting cytokines) are utilized. New types of immune cells either made in the bone marrow, in lymph tissue, or at the specialized skin sites are being discovered for each situation. The local skin tissue has its own memory of immune history and the necessary defenses that were utilized. Microbes, also, can directly influence the skin cells and the immune cells through communication.
The keratinocytes are not at all passive cells, but extremely active in determining both the types of microbes that are allowed near the skin and in calling for the very specific immune cells that are necessary to deal with many different situations. In this elaborate cross talk, hundreds of different cytokines and chemokines (attracting cytokines) are utilized. New types of immune cells either made in the bone marrow, in lymph tissue, or at the specialized skin sites are being discovered for each situation. The local skin tissue has its own memory of immune history and the necessary defenses that were utilized. Microbes, also, can directly influence the skin cells and the immune cells through communication.
Like the intestinal epithelial cells, how can we not say that keratinocytes are very intelligent?

