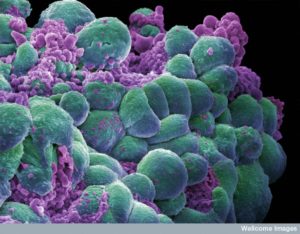
 Cellular communication is ubiquitous in life and previous posts have described many types of cellular languages. Critical signaling occurs in highly complex interactions of bacteria and human cells to help or fight cancer cells in their quest to form their own cellular community. Like other major cellular societies, cancer cells work together to build a tumor and to defend against immune cells, bacteria and viruses that might destroy it. In fact, it is the active interaction with immune cells, bacteria, and critical human barrier cells (intestinal and skin epithelium) that determine the ultimate success of the cancer. A question arises–are microbes friend or foe of cancer? This post will describe the complex interrelationships of these many cells either helping or attacking cancer.
Cellular communication is ubiquitous in life and previous posts have described many types of cellular languages. Critical signaling occurs in highly complex interactions of bacteria and human cells to help or fight cancer cells in their quest to form their own cellular community. Like other major cellular societies, cancer cells work together to build a tumor and to defend against immune cells, bacteria and viruses that might destroy it. In fact, it is the active interaction with immune cells, bacteria, and critical human barrier cells (intestinal and skin epithelium) that determine the ultimate success of the cancer. A question arises–are microbes friend or foe of cancer? This post will describe the complex interrelationships of these many cells either helping or attacking cancer.
Microbes, immune cells, epithelial lining cells and cancer cells, use thousands of different signals—cytokines, neurotransmitters, peptides, protein factors, and RNAs, as well as electric oscillations and fields. Just as the wireless signals that humans send need receivers, each of these cells must produce receptors to understand the signals. Each receives only those messages where genes produce protein receptors and place them into the membranes. Cancer cells must, also, produce all the same signals and receptors.
Bacterial Communication
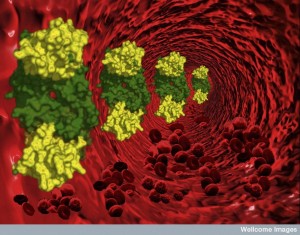
 Previous posts have described the elaborate signaling among bacteria societies, and also their communication with animal and plant cells. With secreted signals, bacteria can immobilize others, kill or eat prey and trigger the formation of large community structures, such as biofilms. Signals can be in the form of proteins injected into a cell using various secretory mechanisms. Proteins can alter cellular scaffolding, membranes, and can directly signal to the genetic machinery of the cell. Microbes and human cells, also, engage in intelligent warfare using specially produced RNAs, and the complex ubiquitin tagging system. Even viruses help or hurt cancers. Bacteria have personal viruses that protect them, and enemy viruses that they constantly battle.
Previous posts have described the elaborate signaling among bacteria societies, and also their communication with animal and plant cells. With secreted signals, bacteria can immobilize others, kill or eat prey and trigger the formation of large community structures, such as biofilms. Signals can be in the form of proteins injected into a cell using various secretory mechanisms. Proteins can alter cellular scaffolding, membranes, and can directly signal to the genetic machinery of the cell. Microbes and human cells, also, engage in intelligent warfare using specially produced RNAs, and the complex ubiquitin tagging system. Even viruses help or hurt cancers. Bacteria have personal viruses that protect them, and enemy viruses that they constantly battle.
Communication Among Human Cells
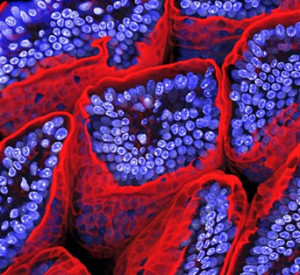 Human cells such as the intestinal epithelial cells, also, have elaborate communication with trillions of microbes in the gut lumen and back and forth signals to the immune system that lies beneath. These cells determine which of the enormous amount of microbes are friendly and helpful and which they will need immune support to defend against. They modulate the immune system below, determining which of the many different immune cells they should send for. They are masters of maintaining order in the midst of chaos. The epithelial cells balance requests from friendly microbes on one side and specific immune cells on the others. The epithelial cells instruct T cells to be tolerant to certain microbes.
Human cells such as the intestinal epithelial cells, also, have elaborate communication with trillions of microbes in the gut lumen and back and forth signals to the immune system that lies beneath. These cells determine which of the enormous amount of microbes are friendly and helpful and which they will need immune support to defend against. They modulate the immune system below, determining which of the many different immune cells they should send for. They are masters of maintaining order in the midst of chaos. The epithelial cells balance requests from friendly microbes on one side and specific immune cells on the others. The epithelial cells instruct T cells to be tolerant to certain microbes.
However, when a normal barrier is broken, such as the lining of the intestine, then microbe and immune cells that fill the void create a new microenvironment that can be helpful to the cancer community. A microbe’s request for protection can alter the environment and increase cancer.
Cancer Cell Signaling
 Cancer cells use all of the complex signals of ordinary human cells, but also defend their community as microbes do. Cancer cells signal each other when viruses attack one of the cells, to warm them to defend themselves. Immune lymphocyte cells have learned how to trigger their metabolism in order to rapidly multiply to fight an infection. Cancer cells use these metabolic innovations from T cells to rapidly alter their own metabolism so the tumor can grow rapidly. Basic metabolic cycles, like the Krebs, are utilized as signals to the genetic machinery to avoid any challenge to their altered reproduction states.
Cancer cells use all of the complex signals of ordinary human cells, but also defend their community as microbes do. Cancer cells signal each other when viruses attack one of the cells, to warm them to defend themselves. Immune lymphocyte cells have learned how to trigger their metabolism in order to rapidly multiply to fight an infection. Cancer cells use these metabolic innovations from T cells to rapidly alter their own metabolism so the tumor can grow rapidly. Basic metabolic cycles, like the Krebs, are utilized as signals to the genetic machinery to avoid any challenge to their altered reproduction states.
Through communication, cancer cells are able to recruit other human cells to help them build blood vessels and an organ structure. They trick immune cells to act as if they are helping to heal a wound and in the process aid the cancer cell. They use cytokines to open blood vessels that make them leaky.
Immune Cell Communication
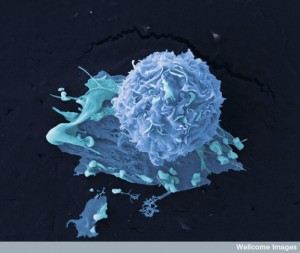
Previous posts have described the very elaborate intelligent behavior of T cells. They communicate through signals and also through direct contact with cells.
 T cells alter their communications for different situations and they are able to totally alter their metabolism to become wildly active and reproductive; in other circumstances they can be quiescent for years remembering how to react to specific possible future invasions. They respond in many different ways to each pattern presented to them, including helping neurons in the brain. They send wireless signals while in the cerebral spinal fluid that stimulates or lowers cognition related to sick behavior in infections.
T cells alter their communications for different situations and they are able to totally alter their metabolism to become wildly active and reproductive; in other circumstances they can be quiescent for years remembering how to react to specific possible future invasions. They respond in many different ways to each pattern presented to them, including helping neurons in the brain. They send wireless signals while in the cerebral spinal fluid that stimulates or lowers cognition related to sick behavior in infections.
But, they can also be tricked into helping cancers. Both microbes and cancer have very complex relationships with immune cells, including elaborate back and forth communications. Immune cells and microbes can fight cancerous cells, but, also, can help them. Modern therapeutic techniques attempt to take advantage of the natural ways that microbes can destroy cancer cells. A small number of microbes have been used to fight cancer for many years.
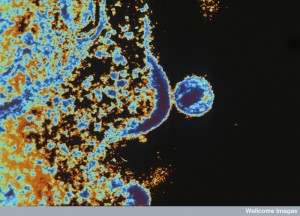
Recently, the poliovirus has been modified to fight a deadly brain cancer, glioblastoma. This therapy is based on the natural ability of poliovirus to invade cancer cells because cancers have an abnormal receptor used for virus entry. For therapy, the virus genes are altered in the laboratory using the splicing of DNA from a common cold virus, which stops the natural dangerous effects of polio. This modified poliovirus kills the cancer cells, but not other normal cells. It doesn’t attack neurons as natural polio does. It, also, creates an immune response that helps destroy the cancer.
Microbes Helping Cancer
 Microbes are considered to be important in the direct or indirect creation of 20% of cancers in humans. Microbes inside of tumors influence the growth and metastasis. The opposite is true as well. Microbes in the gut can decrease inflammation factors and reduce the amount of abnormal cells. Microbes can influence the processes that are involved in human cell reproduction and their destruction. Microbes can promote the effects of the immune system related to cancer cells. Microbes can determine the metabolism of many foods, medications and other chemicals that are related to cancer growth.
Microbes are considered to be important in the direct or indirect creation of 20% of cancers in humans. Microbes inside of tumors influence the growth and metastasis. The opposite is true as well. Microbes in the gut can decrease inflammation factors and reduce the amount of abnormal cells. Microbes can influence the processes that are involved in human cell reproduction and their destruction. Microbes can promote the effects of the immune system related to cancer cells. Microbes can determine the metabolism of many foods, medications and other chemicals that are related to cancer growth.
There are many trillions of different microbe species, but 10 have been found to definitely cause specific cancers in humans. These usually infect a great majority of humans but only cause cancer in a small percentage. Some regions of the human body have vast amounts of microbes, creating very complex environments. These are the surfaces such as the skin (see post The Intelligent Skin Cell), the gut surface (see post The Intelligent Intestinal Epithelial Cells), as well as respiratory and renal surfaces. Many microbes live near the unique environment of the cancer cell without helping the cancer to grow. The opposite can occur when there are fewer of the beneficial protective microbes in a particular environment.
 One way that microbes cause cancer is by helping to move cancer genes into human DNA. Human papillomavirus (HPV) make specific proteins that help cervical cancer. The virus stimulates particular human genes that are helpful to the cancer. Some bacteria have defensive techniques where they damage the DNA of competitors. This can trigger mutations in humans that can lead to cancer. E coli and other bacteria make one particular protein, Colibactin. This molecule, along with several others, has been shown to increase colorectal cancer. It causes breakage of double stranded DNA in cells.
One way that microbes cause cancer is by helping to move cancer genes into human DNA. Human papillomavirus (HPV) make specific proteins that help cervical cancer. The virus stimulates particular human genes that are helpful to the cancer. Some bacteria have defensive techniques where they damage the DNA of competitors. This can trigger mutations in humans that can lead to cancer. E coli and other bacteria make one particular protein, Colibactin. This molecule, along with several others, has been shown to increase colorectal cancer. It causes breakage of double stranded DNA in cells.
Another technique involves proteins that affect basic critical cellular pathways. The Wnt/β-catenin pathway is involved in the function of stem cells and general cellular growth. Several bacteria influence this pathway producing abnormal cancer cells. This pathway can increase the genes for cell multiplication causing gastric and rectal cancers and production of more blood vessels. Another bacterium influences this same pathway to help produce liver cancers. What is surprising is that these bacteria live peacefully in most humans and most situations. Trying to accommodate to a new niche, the bacteria change to have these effects on this vital signaling pathway.
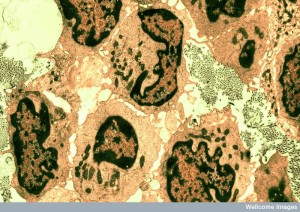
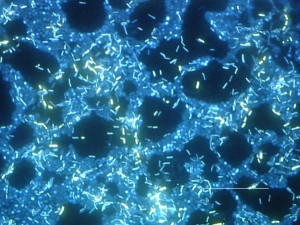 Microbe communities form civilizations of biofilms, which can also help cancers. Colon tumors have associated microbes that form biofilms. Specific regions in the gut appear to be good environments for specific biofilms, which breed tumors. These communities of bacteria are needed to produce the stimulus for the cancer. The individual action is not enough. Several different bacteria produce co metabolites that either stimulate or stop cancer growth.
Microbe communities form civilizations of biofilms, which can also help cancers. Colon tumors have associated microbes that form biofilms. Specific regions in the gut appear to be good environments for specific biofilms, which breed tumors. These communities of bacteria are needed to produce the stimulus for the cancer. The individual action is not enough. Several different bacteria produce co metabolites that either stimulate or stop cancer growth.
Immune Cells, Inflammation and Cancer
 Two previous posts (skin and intestine epithelial cells) described the elaborate communication that occurs between the endothelial barrier cell and the trillions of microbes on one side and the specific immune cells on the other. Under normal conditions, there are constant insults to the barrier and immediate repair by the team of friendly microbes, immune and epithelial cells. Any alteration in the immune response to this constant dynamic situation can lead to abnormal cancerous cells and their spread. When there is destruction of the normal habitat, then microbes and immune cells can be in unusual environments where they do not cooperate any longer. These small regions can produce increased inflammation or the opposite upsetting the balance.
Two previous posts (skin and intestine epithelial cells) described the elaborate communication that occurs between the endothelial barrier cell and the trillions of microbes on one side and the specific immune cells on the other. Under normal conditions, there are constant insults to the barrier and immediate repair by the team of friendly microbes, immune and epithelial cells. Any alteration in the immune response to this constant dynamic situation can lead to abnormal cancerous cells and their spread. When there is destruction of the normal habitat, then microbes and immune cells can be in unusual environments where they do not cooperate any longer. These small regions can produce increased inflammation or the opposite upsetting the balance.
More inflammation can lead to cancer. Inflammation is a dynamic state with movement of many different kinds of cells and elaborate signaling. Most cancers have a microenvironment of low-grade inflammation. This same effect can occur with the metabolic disruption of obesity. In this situation there are more cytokine signals, reactive oxygen and reactive nitrogen creating cancer growth and spread. In fact, cancers develop the ability to increase receptors that will trigger more inflammatory factors. NF-kβ is a very powerful cytokine that can trigger more cancer.
When breaks occur in the normal structures, it allows triggering of immune responses. Many other important cytokines are, also, triggered that produce cancer promoting environments. These include IL-23, IL-17, IL-6, TNF-α.

Microbes are critical factors in inflammation. Microbes are dynamic and change with various situations. A new environment can change helpful microbes into damaging ones. One experiment uses 2 toxins that are damaging to DNA and shows that by breaking a mucosal barrier as well as increasing inflammation, cancer is greatly enhanced. The combination of the disruptions allows rapid transformation of microbes into those that grasp the broken surfaces and invade the tissue. These microbes, also, increasingly trigger cytokines that increase inflammation. All of this aided the transformation and growth of the cancer cells.
Inflammation alters cells to produce different waste molecules including nitrate, which can take on electrons. Microbes shift to provide these electrons and at the same time increase the inflammatory pathways that increase cancer.
The opposite can, also, occur—when a decrease of inflammation increases cancer. Microbes often use systems that stop immune responses to protect themselves . Suppression of immune response is a hallmark of HIV infection and this increases many different cancers related to viruses. The suppression of immune responses by microbes impairs the usual fight against tumors in general. Many treatments for cancer attempt to increase specific immune pathways that fight tumors. Microbes are able to target specific receptors on T cells stopping their anticancer activity.
Metabolic Changes – Microbes, Nutrition, Immunity and Cancer

Ordinarily, microbes help digest fiber in the gut with butyric as a byproduct. Under circumstances of several mutations, butyrate stimulates the creation of new cells and increases transformation to cancer. But, the opposite can occur also. In a different cancer, microbes that associate with the cancer change their metabolism from fatty acid oxidation to glycolysis. This produces butyrate in the cancer cell itself, killing it.
It is still difficult to determine these many relationships, since cancers can develop over many years. Many cancers are not noticed at the beginning and the microbes might have only been helpful to start the cancer cells.
Microbes have many effects in altering the organism’s metabolism, as well as producing byproducts of their own metabolism that have wide ranging effects. Often several metabolites from multiple microbes and the invaded organism interact to produce effects. These often increase or decrease inflammation effects.
Dietary Fibers, Saturated Fats, Microbes, Obesity and Cancer
Various major effects of metabolites occur related to digestion of fiber and saturated fats in the gut; other effects occur with ethanol and estrogens in plant material being digested. Metabolites have wide ranging effects including breaking barriers of the endothelium cells, increasing cell division and planned cell death.
 Microbes in the gut ferment dietary fiber and this produces short fatty acids that have many major effects. (See post on fatty acid signaling in the brain.) Butyrate, acetate and propionate can all produce an environment that produces inflammation. A previous post noted that fatty acids stimulate many different receptors on intestinal and blood cells. Some increase the number of T cells. Some decrease leukemia cells.
Microbes in the gut ferment dietary fiber and this produces short fatty acids that have many major effects. (See post on fatty acid signaling in the brain.) Butyrate, acetate and propionate can all produce an environment that produces inflammation. A previous post noted that fatty acids stimulate many different receptors on intestinal and blood cells. Some increase the number of T cells. Some decrease leukemia cells.
Cancer cells use glycolysis as its metabolic process, which decreases the butyrate and therefore leaves more butryrate in the nucleus of the cells. These higher levels affect modifications on the chromatin by increasing acetyls on the histones causing cell death and decrease of cell division. Butyrate increases cancers by increasing division in epithelial cells.
Particular mutations in cancer drive reactions in different directions. Because of the variation in the results, it is difficult to come up with simple dietary recommendations. One specific metabolite can cause many different effects. While the fiber results show variation, the results of high saturated fats clearly can increase cancer risk. There are complex interactions between the exact diets, the level of obesity, the specific microbes involved, the effects of bile acids and the levels of different kinds of inflammation.
 Obesity is basically a state with increased generalized inflammation. The microbes in the gut have complex relations to obesity. Generally, specific microbes plus inflammation plus obesity is a recipe for cancer. But, studies show that even without obesity, cancer can be stimulated by high fat diet of the wrong kind and specific microbes and inflammation. This occurred in duodenal cancer related to a specific mutation of the endothelial cells. The microbes were altered and transmitted the cancer effects of the high fat diet.
Obesity is basically a state with increased generalized inflammation. The microbes in the gut have complex relations to obesity. Generally, specific microbes plus inflammation plus obesity is a recipe for cancer. But, studies show that even without obesity, cancer can be stimulated by high fat diet of the wrong kind and specific microbes and inflammation. This occurred in duodenal cancer related to a specific mutation of the endothelial cells. The microbes were altered and transmitted the cancer effects of the high fat diet.
Bile acids are supposed to digest fats and allow them to become water-soluble. Microbes produce secondary bile acids. Deoxycholic acid has stimulated cancer, and high fat diets have increased this bile acid, which increases inflammation and cancer. Also, certain mutations that align with obesity do the same thing. This acid increases cell division in liver cells causing liver cancer. Complex relations exist between multiple different cancer mutations, secondary bile stimulation, the microenvironment of obesity and inflammation and specific diets, particularly high fat diet.
Microbes Interact with Cancer Medications
Microbes can increase the amount of a drug causing toxicity and can increase its effectiveness. Most drugs for cancer have a very narrow window just enough to help kill cancer cells, but not enough to kill other cells. Specific microbes produce enzymes that determine the amount of the drug. Therefore, new research is being done into affecting specific bacteria to help with treatment.
Specific microbes, along with immune interactions, determine another agent’s effectiveness. The microbes affect the white blood cells ability to handle oxidative stress. Another agent breaks the gut epithelial barrier, which stimulates microbes to have special T cells to respond. In each type of agent there are very complex interactions between the epithelial cells
Microbes and Immune Therapy for Cancer
 A variety of new immune therapies are now available including use of specific cytokines, antibodies, vaccines against cancer, and targeting specific checkpoint blockades in the sequence of events that trigger immune responses. The situation is very complex, however, because there are many different ways that immune response is stimulated and there are many different microbes that respond in microenvironments in different ways. Examples include the fact that some antibiotics have impaired immune therapies against cancer. Many treatments work best with cancers that aren’t immersed in vast amount of microbes such as exist in the colon.
A variety of new immune therapies are now available including use of specific cytokines, antibodies, vaccines against cancer, and targeting specific checkpoint blockades in the sequence of events that trigger immune responses. The situation is very complex, however, because there are many different ways that immune response is stimulated and there are many different microbes that respond in microenvironments in different ways. Examples include the fact that some antibiotics have impaired immune therapies against cancer. Many treatments work best with cancers that aren’t immersed in vast amount of microbes such as exist in the colon.
New therapies include transplanting white blood cells, which affect the microbes. Many factors have complex interrelationships including the relation of the new blood cells and the old host environment, along with medications and radiation, and the changing environment that occurs with disruption of the barriers. Antibiotics that alter the microbes affect all these. An exiting result is finding a new microbe that restores the ability to fight against clostridium difficile infection using bile acids effects.
Bacteria have elaborate mechanisms to help each other and to kill enemies. New research includes using bacteria to deliver specific toxins to cancer cells.
Microbes alter the effects of immune therapies and chemotherapy for cancer. Gut microbes stimulate reactive oxygen causing DNA damage along with oxalplatin, a specific cancer drug. This stops functioning of DNA and causes cell death. Another drug causes breaks in the lining of the gut, which allows the transformation of bacteria that are in a new environment. In another study antibiotics increased this effect of the microbes.
Are Microbes Friend or Foe of Cancer
 Constant dynamic interaction occurs between the many different communities of cells in the human body. Communication uses many kinds of types of signals and receptors. Ordinary chatter between human cells facilitates their work together in organs. Structural cells, such as fibroblasts, interact with many other cells. Barrier cells, like the gut endothelium and skin, are exposed to vast amounts of microbes and have constant back and forth communication between bacteria, viruses and the wide range of immune cells.
Constant dynamic interaction occurs between the many different communities of cells in the human body. Communication uses many kinds of types of signals and receptors. Ordinary chatter between human cells facilitates their work together in organs. Structural cells, such as fibroblasts, interact with many other cells. Barrier cells, like the gut endothelium and skin, are exposed to vast amounts of microbes and have constant back and forth communication between bacteria, viruses and the wide range of immune cells.
Cancer cells form their own community and set up elaborate communication among all of these other cellular societies. Cancers are now known to be much more variable and dynamic than previously thought, including defending themselves from attacks by virus, bacteria, immune cells and cytokines. Even in a single cancer, there are various cells with different mutations and properties. More and more is being learned about how intelligent cancer cells benefit by signaling with all of these other cells. In the future, finding details of interactions between microbes, immune cells and very unique cancer cells will be critical for treatment.