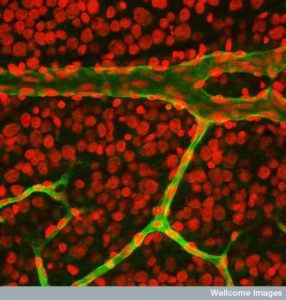
 Conversations among cells are the basis of all life. Important signaling occurs between immune cells, tissue cells, and brain cells. One of the most active and vital type of communication occurs among the cells that form the lining of organs and the matrix cells that form the connective structure.
Conversations among cells are the basis of all life. Important signaling occurs between immune cells, tissue cells, and brain cells. One of the most active and vital type of communication occurs among the cells that form the lining of organs and the matrix cells that form the connective structure.
These wide-ranging discussions include neurons and traveling immune cells, as well. Organs are formed and rebuilt after damage using processes that are part of immune healing activity. There are many similarities to this healing activity involved with limb regeneration in lower animals and inflammation. Both have very active communication among all of these cells, which call for the cells that are needed for various jobs related to building and rebuilding an organ. They involve communication between the lining cells and the connective cells.
Inflammation responses protect against invasion from microbes, and infections, but also protect by helping injuries to heal. Inflammation can also be destructive. The balance between these forces is most difficult at the barrier locations where trillions of microbes interact with lining cells and immune cells—such as the skin, the gut, and the lungs. Please see posts on the intelligent skin and gut cells as background. It is at these regions of intersecting communities of cells where stable structural lining cells (called epithelium or endothelium) converse with more amorphous mobile cells that create a dense supportive matrix (called mesenchymal cells). The latter cell sometimes called connective tissue or stroma has less specific cellular structure, such as cell polarity. It is the conversations among these cells that determines the results of inflammation.
 The immune system is the intermediary between the stationary and traveling cells that react to microbes, injury, and other problems. It provides inflammation for these purposes. This process needs to first be aware of the problem it is asked to solve. It must then call for the necessary supportive cells. It must stop the damaging microbes, cancer, or trauma and then resolve the issue so that more damage doesn’t occur because of the immune cleanup process. Many different back and forth signals promote and inhibit all of these functions. The lining cells and mesenchymal cells are very involved in this communication.
The immune system is the intermediary between the stationary and traveling cells that react to microbes, injury, and other problems. It provides inflammation for these purposes. This process needs to first be aware of the problem it is asked to solve. It must then call for the necessary supportive cells. It must stop the damaging microbes, cancer, or trauma and then resolve the issue so that more damage doesn’t occur because of the immune cleanup process. Many different back and forth signals promote and inhibit all of these functions. The lining cells and mesenchymal cells are very involved in this communication.
Both epithelial lining cells and the more diffuse mesenchymal cells with large matrix are vital to this regulation. Other cells chime in as well, such as neurons, and lymphatics. This post is about the epithelial and mesenchymal conversations. These are vital signals among structural lining cells with connective tissue.
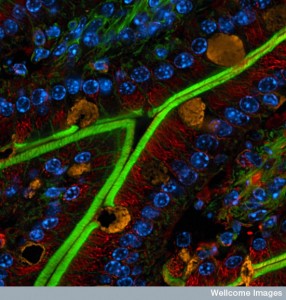
Gut Conversations
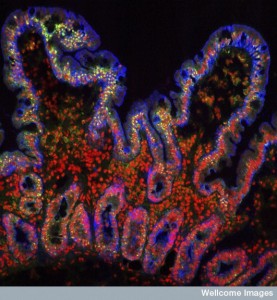 Signals from the gut cells tell the immune system about the types of blood cells that are working their region and their current situation. The long gut has many different types of environments and niches for different types of immune cells and structural stromal cells. Different environments occur in the fast moving center of the flow, the region near the lining cells and protective mucous, and in the deep crypts where stem cells live. These three regions are different all along the small and large intestines.
Signals from the gut cells tell the immune system about the types of blood cells that are working their region and their current situation. The long gut has many different types of environments and niches for different types of immune cells and structural stromal cells. Different environments occur in the fast moving center of the flow, the region near the lining cells and protective mucous, and in the deep crypts where stem cells live. These three regions are different all along the small and large intestines.
Immune cells are often in the specialized lymph tissues both near the surface and deep inside the tissue. Some are Peyer’s patches and others are lymph follicles. These are first created by signals from the mesenchymal cells using a wide range of cytokines (CSCL13, 19, 21, IL-7) and others. These attract cells that induce building the lymph tissues. The stromal cells allow dendritic cells and others to travel easily in the dense tissue with special molecules that they use to attach as they go. Epithelial cells also signal calling for special dendritic cells. B cells are called this way, as well. These attract the largest amount of immune cells in the entire body.
All of these cells signal back and forth to the master T cells. One conversation is about not reacting to food particles with damaging inflammation. Most of the T cells in the tissue are mature cells from the thymus and are looking for particular particles (antigens). The signals are very different along different regions of the large and small intestine. And specific T cells are attracted to each of varied regions.
 Unique microbes in each region are involved in the signals to the T cells. There are multiple different signals in the various layers of one region. Diet particles are important signals in this process. Signals allow cells underneath the border cell to send arms through the dense tight junctions between cells to sample material in the lumen—macrophages and dendritic cells. This allows sampling and protects the barrier function. Signals tell the immune cells which microbes are friendly and necessary for digestion, for example.
Unique microbes in each region are involved in the signals to the T cells. There are multiple different signals in the various layers of one region. Diet particles are important signals in this process. Signals allow cells underneath the border cell to send arms through the dense tight junctions between cells to sample material in the lumen—macrophages and dendritic cells. This allows sampling and protects the barrier function. Signals tell the immune cells which microbes are friendly and necessary for digestion, for example.
Epithelium cells sense action using pattern receptors floating in their membranes and then direct immune responses or the non-action called tolerance. These use a wide variety of cytokines such as IL-10 and 22 directing a wide range of different immune cells. These signals allow epithelial cells to move to places that need reconstruction and healing—resealing broken barriers and surfaces. These signals increase stem cell activities. Other signals stop programmed cell death programs and stimulate other cells. Signals maintain the mucous barrier along with positive and negative signals to friendly and dangerous microbes. The resident cooperative microbes reciprocate with positive return signals.
Conversations tell all the cells to prepare the tissue to go back to normal using regulatory T cells to tamp down the inflammation activity. Often the very lining cells that were damaged let the other cells known to tamp down the activity among all of the immune cells.
Talking About Mucous
 Multiple cells including Goblet cells make mucous barrier molecules (glycoproteins). There are greater amounts of mucous produced in the colon. Without mucous, colitis and cancers occur. Even altering mucous can cause colitis.
Multiple cells including Goblet cells make mucous barrier molecules (glycoproteins). There are greater amounts of mucous produced in the colon. Without mucous, colitis and cancers occur. Even altering mucous can cause colitis.
Because the barrier function is so vital to survival, signals about mucous are central to many pathways related to autophagy, inflammasomes (structures that regulate inflammation processes), and receptor signaling. Signals from the lining cells stimulate and control the special Goblet cells that produce most of the mucous. Conversations among lining cells and microbes, such as parasites, use signals such as allergens and others to determine the amount of the type of mucous that is necessary.
Neurons get into the act. Tuft cells are sensory lining cells producing the signal IL-25 related to interacting with worms. This stimulates other signals that alter the structure of the lining trying to eject the worms. Other conversations are related to how the lining cells are able to work. Signals from the T cells to lining cells triggers increase in the tight junctions and increased barrier function.
Lung Conversations
 Mucous in lungs is thinner than in the gut and is much more mobile. It captures particles and microbes and is moved along by synchronous beating cilia sticking out from the lining cells in the airways. Mucous is produced by goblet cells and club cells and also from ciliated lining cells that provide the cilia beating. These are the two major cells along trachea, bronchi, and bronchioles. Without one type of mucin, macrophages cause inflammation using multiple cytokines such as IL-23. Others cause excess mucous.
Mucous in lungs is thinner than in the gut and is much more mobile. It captures particles and microbes and is moved along by synchronous beating cilia sticking out from the lining cells in the airways. Mucous is produced by goblet cells and club cells and also from ciliated lining cells that provide the cilia beating. These are the two major cells along trachea, bronchi, and bronchioles. Without one type of mucin, macrophages cause inflammation using multiple cytokines such as IL-23. Others cause excess mucous.
An increased number of goblet cells and more mucous are part of increased airway reactivity in allergies from the cytokine IL-13. This sets up signaling that calls for many immune cells to come to the airway—dendritic cells, lymph tissue cells, eosinophils, and T helper 2 cells. Helper T cells produce a viscous cycle of stimulating more goblet cells, mucous, and even more inflammatory cells.
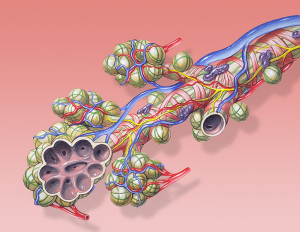
Lining cells have different sets of responses like gut cells. Breathing causes a very large surface area of cells to be exposed to a wide range of unusual particles from the air that include allergens and microbes. Specific responses have been developed for rapid responses to inflammation or to produce tolerance. Some cause decrease of multiple different cytokines that can lower cell destruction and immune response. These can increase allergic reactions. Another set of signals can do the opposite. These two pathways interact and determine the outcomes.
Lining cells also call for specific immune cells as in the gut. Conversations with the immune cells determine the outcome of infection and lung injury (IL-18 and 33). Discussions back and forth are necessary to repair injuries caused by infections such as viral flu.
Likewise signals from the immune cells determine the amount of mucous and the tight junctions between lining cells. They also constitute the extent of the mucous barrier related to damage, and particular inhalation of particles and new allergens. In return lining cells inhibit the extent of the immune response. All of these can cause problems if they are too strong.
Mesenchymal Cells Matrix Barrier
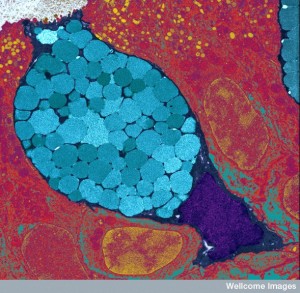
 The strong structural cells and matrix are called connective tissue and hold organs together. The cells that direct this matrix are mesenchymal cells that are more mobile and more amorphous than the more highly structured epithelial cells. Example of the arranged epithelial cells are bipolar type cells where the top, the bottom and the sides look different and have specific different functions. Mesenchymal cells are less structured, more amorphous, and more mobile.
The strong structural cells and matrix are called connective tissue and hold organs together. The cells that direct this matrix are mesenchymal cells that are more mobile and more amorphous than the more highly structured epithelial cells. Example of the arranged epithelial cells are bipolar type cells where the top, the bottom and the sides look different and have specific different functions. Mesenchymal cells are less structured, more amorphous, and more mobile.
Signals from mesenchymal connective tissue cells also regulate immune cells. They also respond to specific signals by altering the matrix structure. Important types of mesenchymal connective cells are often called fibroblasts and myofibroblasts (in muscle) since they make the fiber of the matrix. They also include pericytes, cells that surround blood vessels and make the barrier stronger without being as structured as capillary cells. These different cells have many subsets that are not yet fully recognized. Pericytes are unusual in that they can contract like muscles.
 Connective mesenchymal cells sense and react to any changes in the environment, especially damage, and inflammation. They sense in the same way that immune cells do and adjust the immune environment by sending particular signals.
Connective mesenchymal cells sense and react to any changes in the environment, especially damage, and inflammation. They sense in the same way that immune cells do and adjust the immune environment by sending particular signals.
Mesenchymal connective tissue cells are able to alter their state by going back and forth between stimulating and inhibiting inflammation, like macrophage blood cells. They are constantly talking with lining cells, but differently in each tissue, such as skin, gut, muscle, and lung. It is surprising that there are many different types of connective mesenchymal cells even in the same tissue, such as in the skin where there are many kinds of fibroblasts (papillary, reticular) and they all make different extracellular matrix.
Skin connective cells utilize very unique gene networks involving matrix, growth, types of cells, and memory. Gut cells have many kinds also in different layers—epithelial, crypts, basement membrane, pericytes, lymphatics, lamina propria, and muscularis mucosa.
A recent discovery about cancer is that through conversations among cells, cancer cells attract all supportive cells such as fibroblasts and other connective tissue cells to alter themselves. These supportive cells in the cancer micro environment become essential contributors to the survival of the cancer and ability to travel to form distant metastatic colonies. Connective cells are altered so completely different genetic networks operate allowing them to produce many signals that help the cancer in all phases of life.
Mesenchymal Cells in the Gut
 The connective cells in the gut are very important as sensors and for attracting particular immune cells. They have a wide variety of cytokines and chemokines that call for particular immune cells. They also maintain and keep the immune cells active at the regions where damage has occured or where there is an infection. This stimulation is necessary for the healing to occur and the cleanup. They have many different receptors for different microbes. Surprisingly, they can become cells that present antigens to T cells after bone marrow transplants.
The connective cells in the gut are very important as sensors and for attracting particular immune cells. They have a wide variety of cytokines and chemokines that call for particular immune cells. They also maintain and keep the immune cells active at the regions where damage has occured or where there is an infection. This stimulation is necessary for the healing to occur and the cleanup. They have many different receptors for different microbes. Surprisingly, they can become cells that present antigens to T cells after bone marrow transplants.
Signaling of connective cells can produce dangerous gut inflammation (colitis and cancer) by inhibiting and promoting other cellular conversations. These signals can increase inflammation, but can also increase lining cells and molecules to kill microbes.
Connective cells are vital for repair of injury and infection damage. Both lining cells and connective cells are needed for rehab of injury. However, too much can lead to scars and fibrosis. Damaged lining cells stimulate cytokines that increase connective tissue cells. In lung and kidneys, signals can produce dangerous fibrosis by stimulating fibroblasts to travel, to reproduce, and to produce excessive matrix in between cells. They also attract many other cells such as blood cells, pericytes.
Mesenchymal Cells in the Lung
 Excessive responses of connective cells produce more inflammation in the airways and more mucous secretion. Blood cells are attracted as well. Fibrosis in the lungs can come from these cells around blood vessels and in connective tissue. Pericytes can cause fibrosis in other organs as well, such as kidneys. Pericytes are stem cell like and can become myofibroblasts as well. These vessel cells can attract inflammation to the tissue as well as near the blood vessel.
Excessive responses of connective cells produce more inflammation in the airways and more mucous secretion. Blood cells are attracted as well. Fibrosis in the lungs can come from these cells around blood vessels and in connective tissue. Pericytes can cause fibrosis in other organs as well, such as kidneys. Pericytes are stem cell like and can become myofibroblasts as well. These vessel cells can attract inflammation to the tissue as well as near the blood vessel.
As with other tissues, cancer associated fibroblasts (CAF) have recently been discovered in this and other organs. They engage in many kinds of elaborate communication.
Conversations in Skin
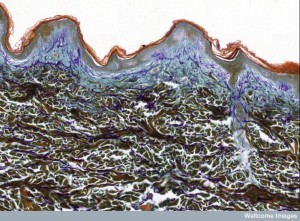 In skin, signals are needed to suppress specific types of inflammation that produce cancers. Special pathways limit signals for the inflammation and cancer. Supportive connective cells in the skin include fat cells that also are part of these conversations. These adipocytes particularly signal to stop Staph aureus infections, producing special peptides, and also to produce more fat cells. Fat cells have elaborate conversations and produce special cytokines that increase special “beige” fat cells. These include the signal IL-33 that supports white fat cells as well.
In skin, signals are needed to suppress specific types of inflammation that produce cancers. Special pathways limit signals for the inflammation and cancer. Supportive connective cells in the skin include fat cells that also are part of these conversations. These adipocytes particularly signal to stop Staph aureus infections, producing special peptides, and also to produce more fat cells. Fat cells have elaborate conversations and produce special cytokines that increase special “beige” fat cells. These include the signal IL-33 that supports white fat cells as well.
Signals can increase energy use that limits the amount of fat tissue that is accumulated. It appears that when damage occurs to the lining epithelial cells in the skin, IL-33 is triggered. Beige fat cells are produced that help regulate immune responses.
Conversations of Lining and Connective Cells
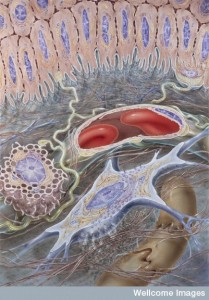 In the fetus, stem cells produce stable structural cells to form organs in exact organizations, and also produce other types of cells that can move and change shape. Later in life a continuum still exists between the stable and more organized epithelial cells and the more amorphous mobile mesenchymal cells. The first forms the border and lining and the second fills in the organ. Both are constantly communicating with all other cells.
In the fetus, stem cells produce stable structural cells to form organs in exact organizations, and also produce other types of cells that can move and change shape. Later in life a continuum still exists between the stable and more organized epithelial cells and the more amorphous mobile mesenchymal cells. The first forms the border and lining and the second fills in the organ. Both are constantly communicating with all other cells.
Recent research has found that the transitions from stable to mobile cells are also vital to develop cancers (the epithelial mesenchymal transitions). These different cells play different roles in the active inflammation for protection and for healing. Conversations between these two types of cells are vital for regulation of immune function as well as all activity in each organ. Each organ has developed different signals and as these are discovered they can possibly be used for new medical treatments.